12.3 Sexual Development
Adolescence begins with the onset of puberty, a developmental period in which hormonal changes cause rapid physical alterations in the body, culminating in sexual maturity. Although the timing varies across cultures, the average age range for reaching puberty is between 9–14 years for girls and between 10–17 years for boys (Marshall & Tanner, 1986). For both boys and girls, these changes include a growth spurt in height, growth of pubic and underarm hair, and skin changes (e.g., pimples). Hormones drive these pubescent changes, particularly the increase in testosterone for boys and estrogen for girls. This chapter will focus on the physical and body chemistry changes associated with puberty. Chapter 14 will expand on these topics as part of more in-depth information on sexual development and topics such as gender identity and sexual orientation.
Sex differentiation, also referred to as sexual differentiation, is the process in which genitals and reproductive organs develop within the womb as a result of complex hormonal processes altering neutral tissues to develop along female and male lines and in which varying combinations are possible as well. Secondary sex characteristics begin to develop further as part of the sex differentiation process during puberty. Therefore, prenatal development, as well as changes that further occur during puberty, create a cascade of events that results in physical changes to the body. Chromosomes, genes, gonads, hormones, and hormone receptor sites play key roles within the endocrine system that influence sex development. Sex is both a genetic and environmental experience in which epigenetic factors can alter the way that genes function, resulting in changes to hormone production and hormone receptor sites at different points across the lifespan.
Puberty is the stage of development at which individuals become sexually mature. Though the outcomes of puberty for boys and girls are very different, the hormonal control of the process is very similar. In addition, though the timing of these events varies between individuals, the sequence of changes that occur is predictable for male and female adolescents. As shown in Figure 12.1, a concerted release of hormones from the hypothalamus (GnRH), the anterior pituitary (LH and FSH), and the gonads (either testosterone or estrogen) is responsible for the maturation of the reproductive systems and the development of secondary sex characteristics, which are physical changes that serve auxiliary roles in reproduction.
The first changes begin around the age of eight or nine when the production of LH becomes detectable. The release of LH occurs primarily at night during sleep and precedes the physical changes of puberty by several years. In prepubertal children, the sensitivity of the negative feedback system in the hypothalamus and pituitary is very high. This means that very low concentrations of androgens or estrogens will negatively feedback onto the hypothalamus and pituitary, keeping the production of GnRH, LH, and FSH low.
As an individual approaches puberty, two changes in sensitivity occur. The first is a decrease of sensitivity in the hypothalamus and pituitary to negative feedback, meaning that it takes increasingly larger concentrations of sex steroid hormones to stop the production of LH and FSH. The second change in sensitivity is an increase in sensitivity of the gonads to the FSH and LH signals, meaning the gonads of adults are more responsive to gonadotropins than are the gonads of children. As a result of these two changes, the levels of LH and FSH slowly increase and lead to the enlargement and maturation of the gonads, which in turn leads to secretion of higher levels of sex hormones and the initiation of spermatogenesis and folliculogenesis.
In addition to age, multiple factors can affect the age of onset of puberty, including genetics, environment, and psychological stress. One of the more important influences may be nutrition; historical data demonstrate the effect of better and more consistent nutrition on the age of menarche in girls in the United States, which decreased from an average age of approximately 17 years of age in 1860 to the current age of approximately 12.75 years in 1960, as it remains today (Martinez, 2020). Some studies indicate a link between puberty onset and the amount of stored fat in an individual. This effect is more pronounced in girls, but has been documented in boys as well. Body fat, corresponding with secretion of the hormone leptin by adipose cells, appears to have a strong role in determining menarche. This may reflect to some extent the high metabolic costs of gestation and lactation. In girls who are lean and highly active, such as gymnasts, there is often a delay in the onset of puberty.
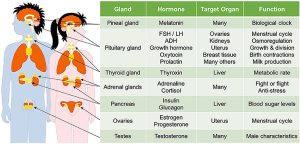 Figure 12.1. There are around 50 different kinds of hormones in the human body. Kabotyanski and Somerville under the terms of the Creative Commons Attribution License (CC BY).
Figure 12.1. There are around 50 different kinds of hormones in the human body. Kabotyanski and Somerville under the terms of the Creative Commons Attribution License (CC BY).
Hormones of puberty during puberty, the release of LH and FSH from the anterior pituitary stimulates the gonads to produce sex hormones in both male and female adolescents.
12.3.1 Signs of Puberty
Different sex steroid hormone concentrations between the sexes in general and within each individual uniquely also contribute to the development and function of secondary sexual characteristics. Examples of secondary sexual characteristics are listed in table 12.1. Each individual’s hormone concentrations will depend upon genetics, diet, stress, and more; thus, secondary sex characteristics will progress along a continuum of possibilities based on these nature multiplied by nurture combinations.
Table 12.1. Development of the Secondary Sexual Characteristics.
|
Female |
Male |
|
|
|
|
|
|
Something to keep in mind as well is that people can experience varying degrees of muscular, breast and hair development depending upon their genetic and environmental makeup. For instance, some boys at the beginning of puberty may see breast tissue growth as well as other body fat increases, and some girls may have facial and body hair growth. One example in this complex process is how unused testosterone is converted to estrogen, for instance, making it not about how much testosterone is present and rather how that testosterone is being used or unused. Also, hormone receptor sites in female cells are often more reactive to lower levels of testosterone. Intersex individuals, females and males all have estrogen and testosterone impacting the changing body during puberty, and it is incorrect to view testosterone as a strictly “male” hormone and estrogen as a strictly “female” hormone. To understand this process, individuals will need to analyze their specific hormone levels, the functionality of genes involved in sex differentiation, and environmental stressors and nutrition that may have epigenetic effects on their genes.
As a girl reaches puberty, typically the first change that is visible is the development of the breast tissue. This is followed by the growth of axillary and pubic hair. A growth spurt normally starts at approximately age 9–11, and may last two years or more. During this time, a girl’s height can increase 3 in. a year. The next step in puberty is menarche, the start of menstruation.
In boys, the growth of the testes is typically the first physical sign of the beginning of puberty, which is followed by growth and pigmentation of the scrotum and growth of the penis. The next step is the growth of hair, including armpit, pubic, chest, and facial hair. Testosterone stimulates the growth of the larynx and thickening and lengthening of the vocal folds, which causes the voice to drop in pitch. The first fertile ejaculations typically appear at approximately 15 years of age, but this age can vary widely across individual boys. Unlike the early growth spurt observed in females, the male growth spurt occurs toward the end of puberty, at approximately age 11–13, and a boy’s height can increase as much as 4 in. a year. In some males, pubertal development can continue through the early 20s.
Hormone blockers for transgender individuals are helpful during puberty to prevent the development of inappropriate secondary sex characteristics that may evoke dysphoria. A concern around hormone blockers is that the parent(s) or guardian(s) are consenting to this treatment on their youth’s behalf, and some caretakers may not feel comfortable with this process. An ongoing debate exists around whether adolescents are mature and aware enough to advocate for themselves. Pediatricians and advocates who are supportive of prescribing hormone blockers and starting hormone replacement therapy express that transgender identities are often expressed during early childhood and remain consistent across the lifespan, whereas others who are against this process tend to express concern over the weight of this decision due to the epigenetic effects of hormone medications that will permanently alter the body and cannot be undone if an individual were to no longer identify as transgender.
12.3.2 Changes based on biological sex assignment
12.3.2.1 Male Anatomy
Males have both internal and external genitalia that are responsible for procreation and sexual intercourse. Males produce their sperm on a cycle, and unlike the female’s ovulation cycle, the male sperm production cycle is constantly producing millions of sperm daily. The male sex organs are the penis and the testicles, the latter of which produce semen and sperm. The semen and sperm, as a result of sexual intercourse, can fertilize an ovum in the female’s body; the fertilized ovum (zygote) develops into a fetus, which is later born as a child.
12.3.2.2 Male reproductive anatomy
Male reproductive anatomy involves the organs and glands that produce sperm, create semen to transport sperm, and conduct this liquid semen out of the body. Semen production involves the work of accessory glands, each responsible for the production of one or more key ingredients of semen. Male anatomical structures can be broken down into the following:
12.3.2.2.1 Sperm production
- Testis: males typically have two testes (also called testicles), which, in humans, descend from the abdomen during fetal development and are enclosed outside the abdomen in the scrotum. Each testis houses many tube-like structures (the seminiferous tubules) in which sperm are made. Specialized cells (the Leydig cells) in the testes produce testosterone.
- Scrotum: a pouch of skin that holds the testes that contracts or expands to adjust the distance the testes are from the body to regulate their temperature (Figure 12.2).
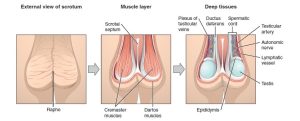
Figure 12.2. External scrotal view: the central raphe on the far left represents the “seam” where the genital tubercles fused in development. In the central image, note the cremaster and dartos muscles, which are important for temperature regulation. On the right, note a deep layer demonstrating the external testes, epididymis, and neurovasculature. Image: “The Scrotum and Testes” by Phil Schatz. License: CC BY 4.0.
- Seminiferous tubules: these structures within the testes are the actual sites of sperm production (discussed further below)
- Epididymis: this rubbery device sits astride the testis. Sperm mature here and are stored prior to ejaculation (when sperm-bearing semen leaves the body, typically during orgasm)
12.3.2.2.2 Semen production
- Seminal vesicles: these two glands produce an alkaline (basic) fluid that can neutralize the acidity of the vagina. This fluid contains fructose and other nutrients to provide energy for the sperm.
- Bulbourethral (or Cowper’s) glands: these two glands provide a mucus-rich alkaline fluid that lubricates the inside of the urethra to allow for easier passage of sperm and neutralizes the urethra (urine residue is acidic). Some of this fluid exits the penis prior to ejaculation (this pre ejaculate fluid can also contain sperm). The remainder of the fluid combines with the semen ejaculate.
- Prostate gland: this organ wraps around the urethra and provides muscular contractions that help propel semen during ejaculation and block urine flow from the bladder during ejaculation. It also provides fluid in the ejaculate that contains enzymes and zinc that aid in sperm motility.
12.3.2.2.3 Sperm/semen transport
- Ductus (or vas) deferens: this pair of muscle-lined tubes carry sperm from the epididymis of each testis into the abdominal cavity where they loop over the bladder and join with the ducts from the seminal vesicles to form the ejaculatory ducts. The muscles that line the ductus deferens contract to propel semen during ejaculation.
- Ejaculatory ducts: these ducts are formed by the joining of the vas deferens with the duct from the seminal vesicle. Each ejaculatory duct empties into the urethra.
- Penis: the organ that encircles the urethra as the urethra exits the abdomen. This organ changes from flaccid (soft and limp) to erect (rigid and standing away from the body) during sexual arousal or spontaneously. In uncircumcised men the penis has a fold of skin called a foreskin that during the flaccid state, covers the head of the penis, and during the erect state retracts behind the glans (or head) of the penis (Figure 12.3).
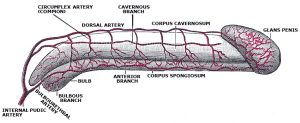
Figure 12.3. Arterial circulation of the penis. “Arterial supply of the penis” by Gray’s anatomy. License: Public Domain.
- Urethra: the tube that runs from the bladder through the penis through which urine and semen exit the body.
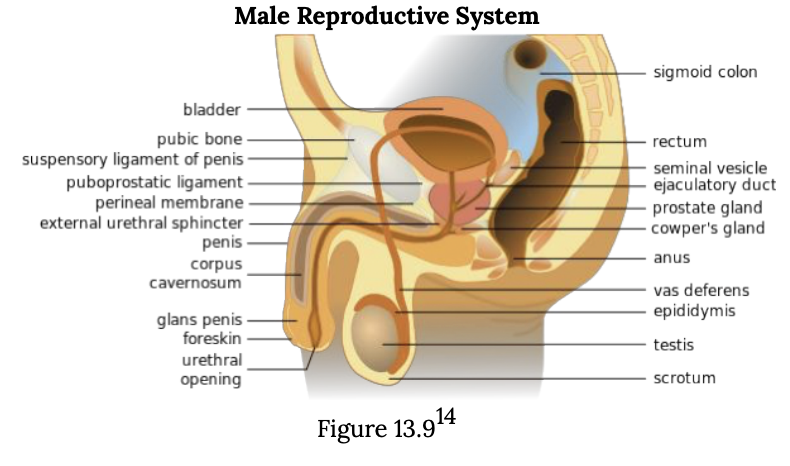
Figure 12.4. Diagram of the male reproductive system.
12.3.2.3 Female Anatomy
Female external genitalia is collectively known as the vulva, which includes the mons veneris, labia majora, labia minora, clitoris, vaginal opening, and urethral opening. Female internal reproductive organs consist of the vagina, uterus, fallopian tubes, and ovaries. The uterus hosts the developing fetus, produces vaginal and uterine secretions, and passes the male’s sperm through to the fallopian tubes while the ovaries release the eggs. A female is born with all her eggs already produced. The vagina is attached to the uterus through the cervix, while the uterus is attached to the ovaries via the fallopian tubes. Females have a monthly reproductive cycle; at certain intervals, the ovaries release an egg, which passes through the fallopian tube into the uterus. If in this transit, it meets with sperm, the sperm might penetrate and merge with the egg, fertilizing it. If not fertilized, the egg and the tissue that was lining the uterus are flushed out of the system through menstruation (around every 28 days).
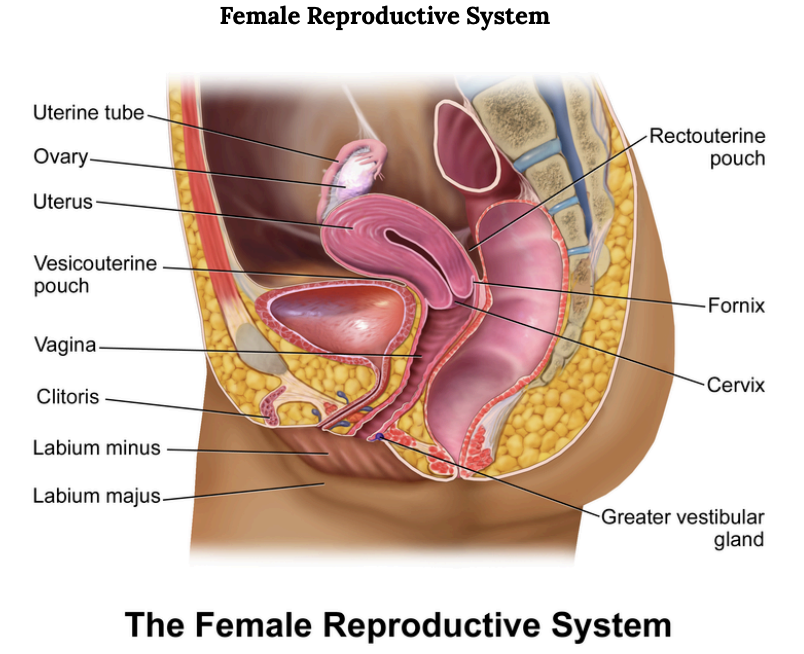
Figure 12.5. Diagram of the female reproductive system.
Some of the organs involved in female reproduction are diagrammed in Figure 12.5. The reproductive structures of the human female are shown.
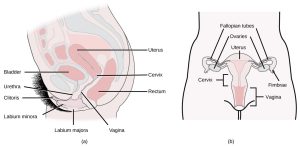
Figure 12.6. Female reproductive anatomy. Credit: modification of work by Gray’s Anatomy; credit b: modification of work by CDC.
The female reproductive anatomy seen in Figure 12.6 includes external structures (the clitoris and vulva), structures involved in the production of eggs and in fetal development (ovaries corpus luteum, and uterus), and structures involved in the transport of sperm, eggs, and babies (vagina, cervix, and oviduct).
12.3.2.3.1 Egg production and fetal development
- Ovary: females have two ovaries that are the site of egg production, and, if an egg is fertilized, the site of the corpus luteum. The ovary produces the hormones estrogen, progesterone, and testosterone.
- Corpus luteum: the site of egg maturation within the ovary. After ovulation (release of the egg) the corpus luteum produces progesterone to maintain a possible pregnancy.
- Uterus: this muscle-lined, triangular organ is where a fertilized egg implants and develops. This organ develops a thick blood lining and sheds this lining on a monthly cycle.
12.3.2.3.2 Transport of eggs, sperm, and embryos
- Vagina: a highly expandable pouch structure that serves as the opening of the female reproductive tract to outside the body. The vagina is the point of sperm entry, and the point of exit for unfertilized eggs, menstrual discharge, and for babies, if pregnant and having a vaginal delivery.
- Cervix: the opening between the vagina and the uterus. The size of this opening varies from tightly closed–to open for the passage of sperm, to open enough for a baby to pass through.
- Oviducts (sometimes called fallopian tubes): these ducts transport mature eggs from the ovary toward the uterus. If a sperm and egg are in the oviduct at the same time, the egg can be fertilized by a sperm.
12.3.2.3.3 Exterior structures
- Vulva: a general term for the exterior parts surrounding the vagina, including the labia majora and labia minora, which are the folds of skin on either side of the clitoris, urethra, and vagina. Often this term is overlooked, with folks referring to the vulva as “vagina,” which is the internal structure. It’s OK and more accurate to say vulva when referring to the external structure. Importantly, the structure and appearance of the vulva may vary widely. There’s no “one size fits all” when it comes to the vulva and diversity in appearance needs to be celebrated.
- Clitoris: the sensitive nerve-rich organ that is analogous to the head of the penis. The part of the clitoris that is visible outside the body is dorsal to (closer to the belly) the urethra and the vagina). The interior part of the clitoris extends internally along either side of the vagina (Figure 12.7).
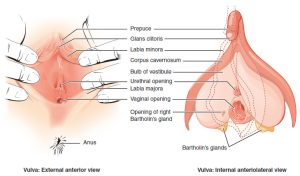
Figure 12.7. Amphis, Public domain, via Wikimedia Commons.
Unfortunately, the structure of the clitoris is not well known by many people, including to those folks with a clitoris. Historically (and even in some contemporary settings), this feature of anatomy has been muted or correlated with antiquated notions of female sexuality such as hysteria or neurosis.
12.3.2.4 Female reproductive physiology
Female reproductive anatomy and physiology has many similarities to that of the male. As described earlier, females also use LH and FSH secretion from the pituitary triggered by GRH from the hypothalamus to stimulate hormone production by the gonads. There is also negative feedback to regulate hormone production. However, in females, the interplay among the hormonal signals is more complicated than in males. While male hormonal feedbacks and signaling provide a relatively steady level of the sex hormone testosterone, for females there is a monthly cycle over which the circulating hormone levels go up and down at the same time as changes occur in the ovaries and the uterus. This surging of hormones along with the changes in the ovaries and uterus require the more complicated physiological controls described below.
12.3.2.4.1 Menstruation
The banner in the picture below was carried in a 2014 march in Uganda as part of the celebration of Menstrual Hygiene Day (Figure 12.8). Menstrual Hygiene Day is an awareness day on May 28 of each year that aims to raise awareness worldwide about menstruation and menstrual hygiene. Maintaining good menstrual hygiene is difficult in developing countries like Uganda because of taboos on discussing menstruation and lack of availability of menstrual hygiene products. Poor menstrual hygiene, in turn, can lead to embarrassment, degradation, and reproductive health problems in females. May 28 was chosen as Menstrual Hygiene Day because of its symbolism. May is the fifth month of the year, and most women average five days of menstrual bleeding each month. The 28th day was chosen because the menstrual cycle averages about 28 days.

Figure 12.8. World Menstrual Hygiene Day celebration by Satirtha—The Helping Hand: a nonprofit organization. CC BY-SA 4.0.
The monthly female reproductive cycle can be divided into three phases, the follicular phase, ovulation, and the luteal phase. For each of these phases, there are concurrent changes happening in the uterus and in the ovaries. See the figure below for a diagram of the phases of the female reproductive cycle and what is happening in the ovary, the uterus, and circulating hormone levels.
12.3.2.4.2 Female hormone cycle
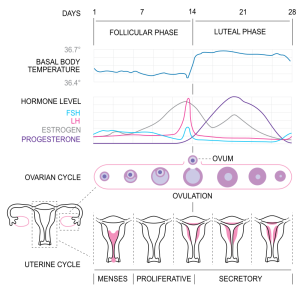
Figure 12.9. Diagram of the menstrual cycle (based on several different sources). CC BY-SA 3.0.
The name “follicular phase” is in reference to the egg-containing follicle in the ovary that matures during this phase (note the ovarian histology shown in Figure 12.9). This phase begins on day one of a female’s reproductive cycle. Day one is defined as the first day of menstruation (the first day of a period). Menstruation occurs for about the first 5 days of the follicular phase. During these days, if a female is not pregnant, low circulating levels of the hormone progesterone trigger the breakdown of the endometrium (the lining of the uterus). This blood-rich tissue exits the uterus through the cervix and then leaves the body out the vagina. During menstruation, low circulating levels of estrogen and progesterone stimulate GnRH production (from the hypothalamus in the brain), which leads to LH and FSH secretion by the pituitary gland. FSH signals the maturation of several follicles within the ovaries. These follicle cells produce a steadily increasing amount of estrogen (note the estradiol (a type of estrogen) increases from day 1–12 in Figure 12.9).
Ovulation refers to the rupture of a mature follicle within the ovary; this ruptured follicle releases an oocyte (an unfertilized egg) into the abdominal space. Because this rupture is an actual breakage, some females will feel a twinge or slight pain during ovulation. Ovulation generally happens around day 14 of the reproductive cycle in one ovary.
During the luteal phase, the now empty follicle within the ovary collapses. This collapsed mass of cells is called a corpus luteum. The corpus luteum produces progesterone that enters the blood circulation. Progesterone signals the hypothalamus to signal the pituitary to reduce FSH and LH production, which prevents other follicles from maturing. If the oocyte in the oviduct is not fertilized, the corpus luteum degrades, causing a drop in progesterone, which triggers the beginning of menstruation and the return to the follicular phase of the reproductive cycle (back to day 1 after about a 28-day cycle). If the oocyte IS fertilized, then that begins the cellular process of fetal development (pregnancy).
12.3.2.5 Intersex Anatomy
About 1 in 1,000–1,500 people will be born noticeably intersex, such as having partial elements of both a penis and vulva. However, other intersex conditions may not show up until later, such as during puberty or when trying to conceive children, making this number higher in actuality. Some estimates show that some intersex conditions can be as high as one in 66. Taken altogether, some researchers, such as Anne Fausto-Sterling (2000), argue that the number of intersex people is actually closer to about one in 100 (Intersex Society of North America, 2008b). Here is a video of four individuals sharing some of their experiences (Figure 12.10).
Figure 12.10. What It’s Like To Be Intersex [YouTube Video].
The term intersex is an umbrella term that encompasses many different variations to sex. Some intersex individuals have variations to their sex chromosomes or that the SRY gene on the Y chromosome is not present or was translocated onto an X chromosome. Thus, in some instances, a male can have XX chromosomes and a female can have XY chromosomes. Other variations are possible as well (X0, XXY, XYY, XXX). According to Dr. Charmian Quigley with the Intersex Society of North America (2008a):
The last time I counted, there were at least 30 genes that have been found to have important roles in the development of sex in either humans or mice. Of these 30 or so genes 3 are located on the X chromosome, 1 on the Y chromosome and the rest are on other chromosomes, called autosomes (on chromosomes 1, 2, 3, 4, 7, 8, 9, 10, 11, 12, 17, 19). In light of this, sex should be considered not a product of our chromosomes, but rather, a product of our total genetic makeup, and of the functions of these genes during development. (para. 11–12)
Therefore, we need to be careful when we oversimplify this process and relate sex to XX or XY chromosomes only.
12.3.2.6 Transgender Anatomy
Further neurobiological research has been conducted to explain why many transgender people experience gender dysphoria, which is an intense feeling that one’s sex assigned at birth based on genital presentation does not match the way they feel about themselves. The contrast between the genital-based presentation of sex and the brain’s sex can be explained from a neurobiology perspective by taking a closer look at sex differentiation when we are still in the womb. During prenatal development, sex differentiation of the genitals takes place during the first two months of pregnancy while sex differentiation of the brain occurs around 4 months of pregnancy (Swaab & Garcia-Falgueras, 2009). This discrepancy between the development of the genitals and the brain has led biological researchers to believe this may be the reason why some individuals are transgender or experience gender dysphoria. Something to keep in mind: Humans actually show a lot less sex dimorphism than many other species, which means that there are actually a lot of similarities between men and women, making this type of research rather difficult as differences are often very subtle if present at all.
Due to the positive results found with treating some transgender individuals using hormone replacement therapy and hormone blockers in order to bring about desirable changes to the physical body, this adds merit to the perspective that there may be some biological reasons and solutions for people experiencing gender dysphoria from a biopsycho perspective. Transgender men: testosterone therapy will result in enlargement of the clitoris leading to resembling a small penis, facial hair and increased body hair similar to other males in the family, redistribution of body fat and increased muscle mass, deepening of the voice due to testosterone thickening the vocal cords, breast tissue will begin to atrophy, and more oily skin. Transgender women: hormone blockers and estrogen hormone therapy will cause breast tissue growth, redistribution of body fat and reduced muscle mass, body hair will thin and grow less fast, penial tissue (if not having regular sex or masturbating) will begin to atrophy, and the skin will become drier. Electrolysis for hair removal may be desired and voice lessons can help train the individual to speak in a more socially expected female register.
Hormone blockers prior to puberty are especially beneficial to prevent these long-lasting impacts and aid the transition process for transgender individuals. Many parents feel conflicted about this, however, and may not consent on their children’s behalf to receive these medical services. Surgeries may also be used by some transgender individuals, commonly referred to within these communities as “top surgery” relating to surgery to either remove or enhance breast tissue or “bottom surgery” on the genitals. Creating a vagina can be done by utilizing the existing tissue and has promising results for many individuals allowing them to experience sensation, but this will depend on scar tissue. Creating a penis will require the addition of testicular implants and a penial pump for erection purposes.
Every transgender person will have to decide what steps they want to take to help them feel as comfortable as possible in their bodies. If someone does not use hormones or have surgeries, it does not make them any less transgender than someone who does. Also, keep in mind that access to healthcare is a privilege and not a right in our country, which can be a barrier for many individuals in receiving the care they need. Family, culture, and society, also act as barriers in this process. It is never appropriate to question a transgender person about their genitals, surgeries or hormones, and doing so would be examples of microaggressions. This is othering and dehumanizing and reduces transgender individuals to their genitals and body rather than seeing them as a whole person with feelings and the right to privacy. Create a space where someone feels comfortable to share their experiences with you on their own rather than questioning them. Here are some resources:
- National Center for Transgender Equity.
- Trans Student Educational Research.
- Supporting the Transgender People in Your Life: A Guide to Being a Good Ally.
Additional resources for your reference: If you or someone you know is interested in learning more about how hormone replacement therapy impacts the body, check out the links provided by the University of California San Francisco Transgender Care. UCSF Transgender Care also has more information on the types of surgeries that are available for transgender individuals.
What about when nonbinary individuals, such as those who identify as agender, bigender, genderqueer, among others, and experience gender dysphoria as well? Or, what about when transgender individuals don’t experience gender dysphoria? What might be some biological explanations? We need more research! A question to think about further: if gender is a social construct, then does biology even really matter anyway and are researchers trying too hard to find biological answers? This goes back to the nature/nurture debate once again. We will discuss gender as a social and cultural phenomenon next week to explore this question further from other perspectives.
12.3.3 Licenses and Attributions for Sexual Development
Introduction to Human Sexuality by Ericka Goerling, PhD and Emerson Wolfe, MS is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License, except where otherwise noted.
