12.4 Sexual activity
12.4.1 Pregnancy
Although adolescent pregnancy rates have declined since 1991, teenage birth rates in the United States are higher than most industrialized countries. In 2020, females aged 15–19 years experienced a birth rate of 15.4 per 1,000 women (Martin et al., 2020). This is a drop of eight percent from 2019. It appears that adolescents seem to be less sexually active than in previous years, and those who are sexually active seem to be using birth control.
12.4.1.1 Risk Factors for Adolescent Pregnancy
Miller et al. (2001) found that parent/child closeness, parental supervision, and parents’ values against teen intercourse (or unprotected intercourse) decreased the risk of adolescent pregnancy. In contrast, residing in disorganized/dangerous neighborhoods, living in a lower SES family, living with a single parent, having older sexually active siblings or pregnant/parenting teenage sisters, early puberty, and being a victim of sexual abuse place adolescents at an increased risk of adolescent pregnancy.
12.4.1.2 Consequences of Adolescent Pregnancy
After a child is born life can be difficult for a teenage mother. Only 40 percent of teenagers who have children before age 18 graduate from high school. Without a high school degree, her job prospects are limited and economic independence is difficult. Teen mothers are more likely to live in poverty and more than 75 percent of all unmarried teen mothers receive public assistance within 5 years of the birth of their first child. Approximately, 64 percent of children born to an unmarried teenage high-school dropout live in poverty. Further, a child born to a teenage mother is 50 percent more likely to repeat a grade in school and is more likely to perform poorly on standardized tests and drop out before finishing high school (March of Dimes, 2012).
12.4.2 Sexually transmitted Infections
Sexually transmitted infections (STIs), also referred to as sexually transmitted diseases (STDs) or venereal diseases (VDs), are illnesses that have a significant probability of transmission by means of sexual behavior, including vaginal intercourse, anal sex, and oral sex. It’s important to mention that some STIs can also be contracted by sharing intravenous drug needles with an infected person, through childbirth, or breastfeeding. Common STIs include:
- chlamydia
- herpes (HSV-1 and HSV-2)
- human papillomavirus (HPV)
- gonorrhea
- syphilis
- trichomoniasis
- HIV (human immunodeficiency virus) and AIDS (acquired immunodeficiency syndrome)
According to the Centers for Disease Control and Prevention (CDC) (2023), there was an increase in the three most common types of STDs in 2021. Those most affected by STDs include racial and ethnic monitories, adolescents and young adults, and men who have sex with men. The most effective way to prevent transmission of STIs is to practice abstinence, (not participating in sexual intercourse), safe sex, and to avoid direct contact of skin or fluids which can lead to transfer with an infected partner. Proper use of safe-sex supplies (such as male condoms, female condoms, gloves, or dental dams) reduces contact and risk and can be effective in limiting exposure; however, some disease transmission may occur even with these barriers.
12.4.3 Contraceptive Methods and Protection from Sexually Transmitted Infection
There are many methods of contraception that sexually active adolescents can use to reduce the chances of pregnancy (table 12.2 and Figure 12.11).
Table 12.2. Contraception Methods.
|
Method |
Description |
Failure Rate |
|
Intrauterine Contraception (IUD) |
An IUD is a small device that is shaped in the form of a “T” placed inside the uterus |
0.1–0.8% |
|
Implant |
A single, thin rod that is inserted under the skin of a woman’s upper arm |
0.01% |
|
Injection |
Injections or shots of hormones to prevent pregnancy are given in the buttocks or arm every three months. |
4% |
|
Oral contraceptives |
Also called “the pill,” contains the hormones to prevent pregnancy. A pill is taken at the same time each day. |
7% |
|
Patch |
This skin patch is worn on the lower abdomen, buttocks, or upper body and releases hormones to prevent pregnancy into the bloodstream. A new patch once a week for three weeks and then left off for a week |
7% |
|
Hormonal vaginal contraceptive ring |
The ring is placed in the vagina and releases the hormones to prevent pregnancy. It is worn for three weeks. A week after it is removed a new ring is placed. |
7% |
|
Spermicide |
These kill sperm and come in several forms—foam, gel, cream, film, suppository, or tablet. They are placed in the vagina before intercourse. |
21% |
|
Diaphragm or cervical cap |
A cup that is placed inside the vagina to cover the cervix to block sperm. It is inserted with spermicide before sexual intercourse. |
17% |
|
Sponge |
This contains spermicide and is placed in the vagina where it fits over the cervix. |
14–27% |
|
Male condom |
Worn (single use) by the man over the penis to keep sperm from getting into a woman’s body. |
13% |
|
Female condom |
Worn (single use) by the woman inside the vagina to keep sperm from getting into a woman’s body. |
21% |
|
Natural Family Planning |
During a regular menstrual cycle, fertile days can be predicted. Sexual intercourse can be avoided on those days. |
2–23% |
|
Copper IUD |
Can be inserted up to 5 days after sexual intercourse |
0.8% |
|
Emergency contraceptive pills |
Can be taken up to 5 days after sexual intercourse and may be available over-the-counter |
1–10% |
In choosing a birth control method, dual protection from the simultaneous risk for HIV and other STIs also should be considered. Although hormonal contraceptives and IUDs are highly effective at preventing pregnancy, they do not protect against STIs, including HIV. Consistent and correct use of the male latex condom reduces the risk for HIV infection and other STIs, including chlamydial infection, gonococcal infection, and trichomoniasis.
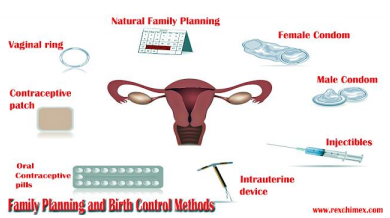
Figure 12.11. Image by rexchimex is licensed under CC BY 4.0.
12.4.4 Licenses and Attributions for Sexual activity
“Sexual Development” by Terese Jones is licensed under CC BY 4.0.
