7.2 Mental Health and Connection to Human Services
Like many of the topics in this text, mental health is a subject in which you will need to be well-versed in order to be a professional working in human services. Clients are usually dealing with some sort of adversity in their lives, and those circumstances can take their toll on mental health. Struggling with mental illness can also cause a ripple effect of other problems in one’s life—work or school performance issues, relationship problems, substance use, medical problems, and more.
Even if you do not plan to be a clinical social worker, counselor, or someone otherwise employed in the mental health field, it is imperative that you feel comfortable working with clients with mental health challenges. You will need to be able to recognize the signs and symptoms of many disorders so that you can help clients connect to the resources that can best assist them. Clients who are struggling with their mental health may not be able to work toward goals in any human services program until those needs are addressed or at least recognized.
This chapter is an introduction to some of the settings and problems you may encounter. Most importantly, we understand practitioners’ ethical scope of practice in the human services field with our skill set and training, as we want to help and not harm the communities we serve.
What Are Mental Health Disorders, Mental Health, and Mental Wellness?
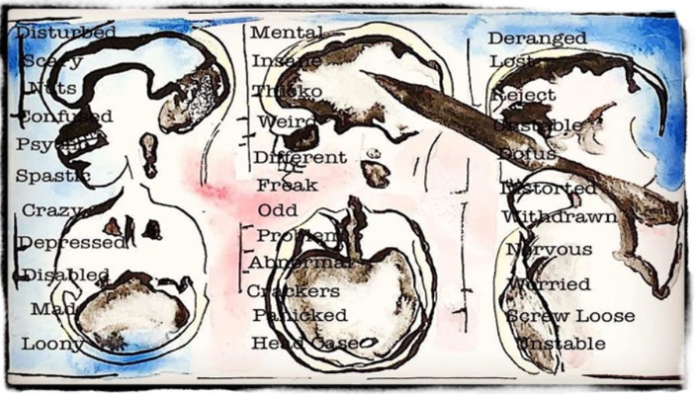
We have come a long way in the terms we use for various psychiatric conditions, though we continue to modify our terminology seemingly at every step. However, it is not unusual for people still to use words like “crazy,” “unbalanced,” “nuts,” “out of it,” “psychotic,” and “insane” to describe those who are dealing with mental disorders. These words reflect many things: misunderstanding, fear, misinformation, miseducation, and more.
Many people do not have a firm understanding of mental health disorders. It is easier to think in hurtful terms like these to describe those who are dealing with mental disorders. As human service providers, we must advocate and educate not just clients and their families but also colleagues, family, and friends about these words and topics that will help reduce the stigma around mental health disorders, as depicted in figure 7.1.
You may hear the terms “mental illness” and “mental disorder” used interchangeably, and there isn’t necessarily anything wrong with that approach. The Diagnostic and Statistical Manual of Mental Disorders (Fifth Edition-Text Revision), commonly called the DSM-5TR, uses the term mental health disorder to describe psychiatric diagnoses, and that is what we will use in this text. The DSM-5’s definition of mental disorder is as follows: “A syndrome characterized by clinically significant disturbance in an individual’s cognition, emotion regulation, or behavior that reflects a dysfunction in the psychological, biological, or developmental processes underlying mental functioning” (American Psychiatric Association [APA], 2022).
This is something they (mental health providers) have received unique and specific training to do. Human service providers will not be asked to diagnose clients in the field. Do not assume anyone’s diagnosis or see someone’s symptoms and think, “I know what they may have as a diagnosis.” If you do not have the training and experience to do so, then do not diagnose anyone. It is unethical and outside the scope of your practice to do so.
Some people feel that the term “mental illness” sounds too negative and may stigmatize people who have been diagnosed with mental disorders. Others are dismayed by the word “disorder” and what it implies about their functioning state. Plus, we have not yet considered intergenerational trauma and the centering of Western medical perspectives of what health and healing looks like.
If you won’t be providing a diagnosis to clients, why should you be aware of the definition of a mental health disorder? Not only for advocacy and to help reduce the overall stigma of mental health disorders but because we cannot separate the human experience from the prevalence of mental health disorders you will encounter while working in the field. These disorders are common, and human services professionals must understand how various client needs will impact your approach to your work.
What about the terms mental health and mental wellness? First, humans have one thing: mental health. Mental health is a state of mind characterized by emotional well-being, reasonable behavioral adjustment, relative freedom from anxiety and disabling symptoms, and a capacity to establish constructive relationships and cope with life’s ordinary demands and stresses” (American Psychological Association, 2018, para. 1). Mental wellness is an “internal resource that helps us think, feel, connect, and function; it is an active process that allows us to build resilience, grow, and flourish” (Global Wellness Institute, 2020, para. 1).
How Common Are Mental Health Disorders?
As with many important topics, the available statistics on the prevalence of mental disorders vary. The Substance Abuse and Mental Health Services Administration (SAMHSA) reports that 33.7% of adults qualified for a mental disorder diagnosis in 2021; about one in four of those disorders (16%) would be classified as severe. In the 2022 National Healthcare Quality and Disparities Report, almost 20% of children and young people ages 3–17 in the United States have a mental, emotional, developmental, or behavioral disorder, and suicidal behaviors among high school students increased by more than 40% in the decade before 2019. Mental health disorders were the leading cause of death in this age group. These trends were exacerbated during the COVID-19 pandemic, which is not a surprise as it magnified the needs many have had for years. However, it (mental health needs) has not been highlighted or seen as necessary or as many people could not slow down enough to notice.
In order to assess these numbers, we need to consider how, as a society, we look at mental health disorders from a gendered view and a racial lens. We need to understand how intersectional identities impact who is receiving mental health referrals for support and possible diagnosis. We also need to think about how our own biases play into the way we interact with clients who may have mental health disorder diagnoses, even if we only suspect they’ve been diagnosed.
What Can Be Done to Support People with Mental Health Disorders?
This chapter will delve into some of the many different options available to people with mental disorders—both medications and various kinds of therapy and counseling. Although there are many disorders, there are also a lot of clinicians with expertise in a broad range of areas, as well as plenty of research to show how to handle particular issues. Though mental disorders can be difficult, upsetting, or even scary in some situations, there is plenty of reason to have hope for recovery and improvements in functioning.
Having a basic understanding of mental health and mental disorders will increase the effectiveness of any human services practitioner. What is essential to understand is the scope of our practice and what we can do in our role. Suppose we are a peer support provider or a home visitor. In those cases, we understand our role limits and know that we are not the ones who will be providing the clinical mental health support directly related to diagnosing the disorder. Instead, we will be providing resources to support the symptoms we observe and that clients report as impactful to their lives or to help construct a treatment plan. We could help locate and build a community and network with families.
We can skillfully create a space of empathetic listening and care for clients without providing clinical treatment. One of the most supportive things we provide is learning how to be with someone but trying to fix something about them or their situation. The relationship is the center of everything, first and foremost. Building trust is critical.
Licenses and Attributions
“Mental Health and Connections to Human Services” is adapted from “Mental Health and Treatment” in Social Work & Social Welfare: Modern Practice in a Diverse World by Mick Cullen and Matthew Cullen, and is licensed under CC BY 4.0. Adaptations by Elizabeth B. Pearce: Minor editing for clarity; shortened sections and elimination of some disorders; updated; refocus of content on to human services. Revised by Martha Ochoa-Leyva.
Figure 7.1. “Crazy Brain” by William Doan is licensed under CC BY ND 4.0.
a professional field focused on helping people solve their problems.
results from an event, series of events, or set of circumstances that is experienced by an individual as physically or emotionally harmful or life threatening and that has lasting adverse effects on the individual’s functioning and mental, physical, social, emotional, or spiritual well-being

