9.6 End of Life, Dying, and Supports
Death is something that is not an easy topic for many and taboo for others to bring into a conversation. It is usually only talked about as we are getting older, especially in the United States. Conversations around death are deemed “inappropriate,” and unnecessary for many in this country, since it is “supposed” to take place later due to advances in technology and medicine. However, this also denies many people the ability to fully understand what living is because so much fear surrounds what death looks and feels like.
Many people have spiritual, religious, and even scientific ideas of what happens after we die, but we are advocating for more openness about starting conversations and supporting this topic. Cultures around the world have thousands of years of practice with open conversation around death from the very start of life, and it is not something that is seen as inappropriate to talk about or a taboo subject. These conversations are not age-restricted, since they are not connected to fear but to how the whole culture lives.
Cultures all around the world, from Mexico to Africa, have practices around death that are different and open in comparison to the United States. This section will help you as practitioners consider how this field of human services and social work intertwines with conversations to support communities around death, dying, and grief.
Death with Dignity Act
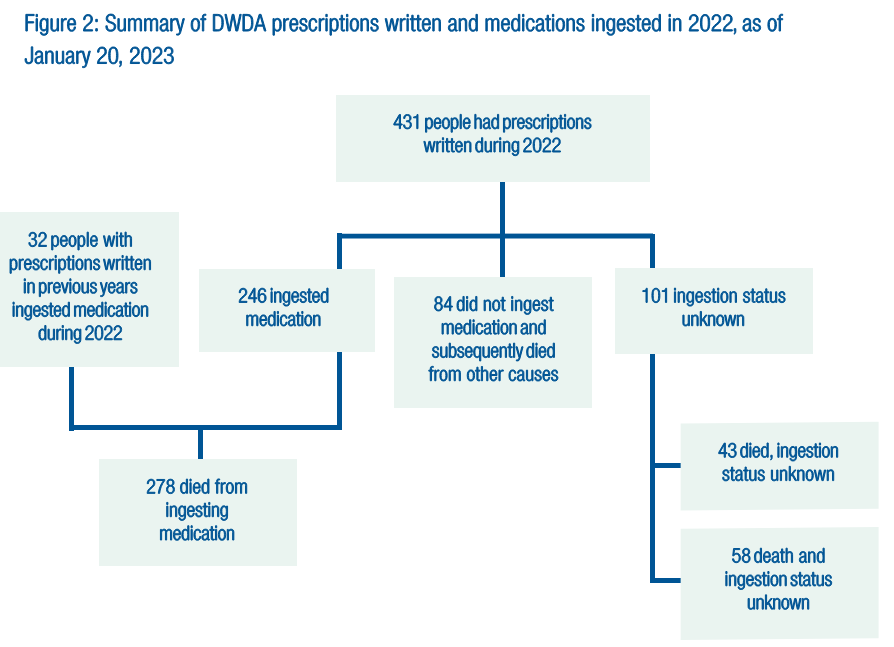
Oregon enacted the Death with Dignity Act (DWDA) on October 27, 1997. It allows terminally ill individuals to end their lives through the voluntary self-administration of lethal medications expressly prescribed by a physician for that purpose after meeting clearly defined criteria outlined in the law, including safeguards. Outcomes for the 2022 enrollees in the DWDA program are visualized in figure 9.14. You can optionally read the complete law linked at Oregon’s Death with Dignity Act [Website]. The criteria for eligibility are as follows:
1) Must be 18 years of age or older.
2) Must be capable of making and communicating health care decisions to health care practitioners.
3) Must be diagnosed with a terminal illness that will lead to death within six months.
The attending and consulting physicians must determine whether a patient meets these requirements and report that fact to Oregon Health Authority (OHA) at the time a prescription is written. When OHA identifies any instance of noncompliance with the statutory requirements, it reports the instance to the appropriate licensing board.
In October 2021, a lawsuit was filed against the state of Oregon alleging that the residency requirement in the act violated the Privileges and Immunities Clause and the Dormant Commerce Clause of the United States Constitution. This prevented Oregon health care providers from offering medical aid to dying nonresident patients. The case was presented in the U.S. District Court for the District of Oregon, and on March 28, 2022, a settlement was reached. As per the agreement, the state would not enforce the residency requirement mentioned in the act and would introduce a legislative concept to repeal the residency requirement in several sections.
I understand that it is a sensitive topic, and it’s important to note that a patient’s state of residence is not collected during the DWDA prescription process. OHA only receives death certificates from other states if the deceased was an Oregon resident; therefore, if an Oregon DWDA patient dies out of state and is not an Oregon resident, it’s unlikely that OHA will be informed of the death. As a result, the out-of-state deaths reported may not represent all DWDA deaths from out-of-state residents who received a DWDA prescription from an Oregon health care provider.
It’s important to understand that the changes made to the act were to ensure that all individuals receive the care they deserve regardless of their residency. The Oregon Legislative Assembly passed House Bill 2279, removing all text in the act related to the residency requirement for patients receiving medical aid in dying. This was done in hopes that it would bring some peace of mind to those who were affected by the previous requirement.
As providers in the field, we may struggle with the idea of suicide and our own personal beliefs around it. But many people are going to need our support during times of great need, which can include moments near the end of life or when members of a client’s family have decided to use something like DWDA. Understanding what this act means and how we can support clients is important both for our own growth and our clients’ needs. If a client has decided they want to move forward with this, there is additional support available.
End of Life Doulas
The idea of supporting someone entering this world with a birthing doula is well known by many and used in many cultures around the world. So are end-of-life doulas. The work of end-of-life doulas is described by International End of Life Doula Association (INELDA):
End-of-life doulas provide companionship, comfort, and guidance to those facing a terminal illness or death. Our non-medical holistic support encompasses emotional, spiritual, and practical care. We offer resources to help the dying person, along with their family and loved ones, make informed decisions in a supportive environment.
A doula can become involved any time in a person’s life. We offer support when people are impacted by a life changing illness, after a terminal diagnosis, when death is imminent, or even after a death—to help with light grief support. Sometimes family members or loved ones of the person dying seek support and guidance from end-of-life doulas.
Doulas normalize deathcare by creating spaces to hold conversations leading to increased communication and increased spiritual and emotional well being. When individuals plan for death, they have autonomy over their decisions and are able to clearly define their end-of-life wishes with family and loved ones. While there are alternative names for end-of-life doulas like death doula, death midwife, death coach, end-of-life coach—we all seek to provide compassionate deathcare. (International End of Life Doula Association, 2023)
This is a career that many people are unaware of as being a possibility. It is a way to work with aging adults and their families with compassion. It centers their humanity and needs by combining medical, social services, cultural, and spiritual supports in a unique, client-centered way.
Licenses and Attributions
“End of Life, Dying, and Supports” by Yvonne M. Smith LCSW is licensed under CC BY 4.0. Revised by Martha Ochoa-Leyva.
Figure 9.14. Figure 2: Summary of DWDA prescriptions written and medications ingested in 2022, as of January 20, 2023 by Public Health Division, Center for Health Statistics, is included under fair use.

