4.2 Criminalization of Mental Disorders
Perhaps Jamie, described in the chapter overview, is soon released from custody – without resolution of housing issues, medical and psychological problems, or substance use; without increased access to healthcare and medications; and with a new legal barrier: criminal charges. Or, alternatively, Jamie is too mentally ill to even understand what has happened, so Jamie stays in jail awhile longer, awaiting an evaluation and some legal negotiations. At this point, Jamie still has not resolved any existing issues, likely has exacerbated mental health symptoms, and is sitting in custody. The criminal justice system has been employed to address real problems, but it has arguably made these problems worse. Most of us can, also, imagine far worse outcomes for Jamie and the community when armed police respond to this type of situation. Jamie’s story is just one example of the problem of criminalization (figure 4.1).

Figure 4.1. A person sits alone, locked in a jail cell. Criminalization of mental disorders can exacerbate pre-existing problems of isolation and mental illness for people who are arrested.
The criminalization of mental disorders refers to the use of the criminal justice system as the first-line response for people who come to the attention of authorities primarily due to their mental disorders and then face criminal justice consequences such as arrest, criminal charges, and incarceration. As in the chapter-opening scenario with Jamie, criminal justice consequences can escalate once they get started. And, because the criminal justice system can be ill-equipped or unable to resolve cases involving serious mental health issues, people can remain “stuck” in the system for much longer than expected or intended. While stuck, a person with mental disorders may find that their original mental health condition deteriorates, or makes them subject to victimization or self-harm.
Of course, people who have mental disorders do commit offenses, of all levels of seriousness, that warrant criminal processing. But the problem of criminalization we consider here arises when people are not, primarily, criminal in their conduct but are brought into the criminal justice system and criminal treatment worsens the situation. A person may have done something that is technically offending behavior (as in Jamie’s case), or community members may legitimately fear that a person will engage in increasingly offensive behavior due to obvious signs of mental illness. Police are then enlisted to assist, usually as the only response option available, and the person is then introduced (or re-introduced) into the criminal justice system. Oftentimes, this person is not dangerous and primarily needs help. They do not need or benefit from criminal processing, and in fact they and the larger community may be harmed by this response.
4.2.1 The Roots of Criminalization
As discussed in Chapter 1 of this text, the deinstitutionalization movement – eliminating long-term hospitalizations in favor of community support for those with mental disorders – began in the early 1960s with high hopes, but more moderate accomplishments. The righteous intent of deinstitutionalization was to eliminate the incarceration and segregation of people with mental disorders, and to provide help and treatment to this population in their communities.
The planned reduction of institutions became a reality: from 1955 to 1975, the number of people committed to institutions had dropped from around 550,000 to 200,000, and counts would continue to plummet in upcoming decades, even as the population overall increased (Substance Abuse and Mental Health Services Administration, 2019). Hundreds of thousands of people with mental disorders were leaving hospitals to live in the community, as was their right. While this staggering reduction of institutionalization had been the precise goal of impacted individuals, civil rights advocates, lawmakers and taxpayers, the next steps in the deinstitutionalization movement did not fully materialize.
Despite the reduction of people with mental disorders in state hospitals, there was an inadequate corresponding increase in community-based support. The planned community health centers were only partially completed. And mental health care was simply not available at the level of demand. Most health insurers didn’t cover mental health – or certainly not at the level they covered other physical health conditions – until that was demanded by law in 2010 under the Affordable Care Act. For many, this law came decades too late. Many of the people released from restrictive hospital settings properly re-entered the community but had no real chance of succeeding there.
The gap in support that grew after deinstitutionalization led to a newly voiced concern by observers beginning in the 1970s: the criminalization of those with mental disorders. And indeed, many of those who had been released from closing institutions fell into the gap in care, and they were wholly unable to meet their basic needs. They ended up in jail or prison, with the criminal justice system providing the “care” that was unavailable elsewhere. To some, it appeared that people with mental disorders were simply going to be shifted from one institution to another: from state hospitals into prisons.
But the increase in incarcerated people with mental disorders was not due to closure of institutions alone, by any means (Lurigio, 2013). Another enormous factor was the overall increase in incarceration generally, and particularly the increase due to drug-related convictions. The United States was getting “tough on crime,” especially drug offenses. President Richard Nixon’s “war on drugs” in 1971 gained speed and power in the 1980s and continued for decades – imposing draconian prison sentences at both the state and federal level. In 1950, 175 out of every 100,000 United States residents were incarcerated. By 1985, the number was up to 312 per 100,000 and rising. By 2005, it was at 743 per 100,000 (Cullen, 2018).
Women were a significant part of the increase in incarceration, especially women of color. From 1990 to 2010, the number of women in prison increased twice as fast as the rate for men; of those, Black women were more than three times as likely as white women to be incarcerated. Most of the women in prison are mothers of young children – creating complicated family struggles (Lapidus, 2011). There was also an enormous impact on people with mental disorders, who often experience primary or co-occurring substance use disorders as part of their diagnosis. Drug use leads to an increase in criminal system engagement for most people, and especially for people with serious mental illness (Lurigio, 2013).
4.2.2 Criminalization Today
Some fifty years after concern about criminalization was first voiced, the problem has grown and persists. People who experience mental disorders are vastly overrepresented in our nation’s jails and prisons, especially among vulnerable populations including youth, women, and veterans (National Alliance on Mental Illness, 2022). Stigma around mental illness and disability, and the inaccurate assumption that people who have mental disorders are very likely to engage in criminal activity, continues to fuel the practice of treating mental disorders as a criminal justice issue (Pescosolido et al., 2019).
The rate of mental disorders among incarcerated people began to rise in the 1970s and kept going up – now appearing at a rate up to 12 times that found in the general population (Wolff, 2017). Nearly all states have more patients with mental disorders in their jails and prisons than they hold in state hospitals. According to the non-profit Treatment Advocacy Center, people experiencing serious mental illness such as schizophrenia are ten times more likely to be in a jail or prison than in a hospital (Treatment Advocacy Center, n.d.). About half of the people incarcerated in Oregon prisons, for example, have diagnosed mental illnesses and/or developmental disabilities (Oregon Health Authority, 2018). The Cook County Jail in Chicago, widely reported to be the largest mental health facility in America, is full of people who have mental illness and have committed so-called “crimes of survival” – theft to get something to eat, breaking and entering to find a place to sleep (Ford, 2015).
People living in extreme poverty, namely the houseless population, are at serious risk of experiencing criminalization due to mental disorders, including substance use disorders. Though Portland, Oregon is not unique, statistics from this one city provide a snapshot of how these issues manifest. In 2017, more than half of Portland Police Bureau arrests involved people living on the street. The approximately 10,000 arrests of homeless people that year were most often based on low-level crimes such as theft or drug charges; 86% of the arrests were for non-violent crimes, with more than 1200 of the arrests involving procedural offenses such as missing court (Woolington & Lewis, 2018).
For many probable reasons, led by lack of robust mental health care, there is not a clear accounting of exactly how many of Portland’s homeless arrestees have diagnosed mental disorders, but evidence suggests the numbers are high. The homeless population overall is far more likely than others to be affected by mental disorders (figure 4.2). Almost half of Portland’s homeless residents overall self-report themselves as having mental illness; 38% report physical disabilities; and another 37.5% report substance use issues (Maui, 2019). Disability is more common than not among homeless residents of Portland generally, with higher numbers in certain groups: 67% of homeless women, for example, self-identify as disabled (City of Portland, n.d.).
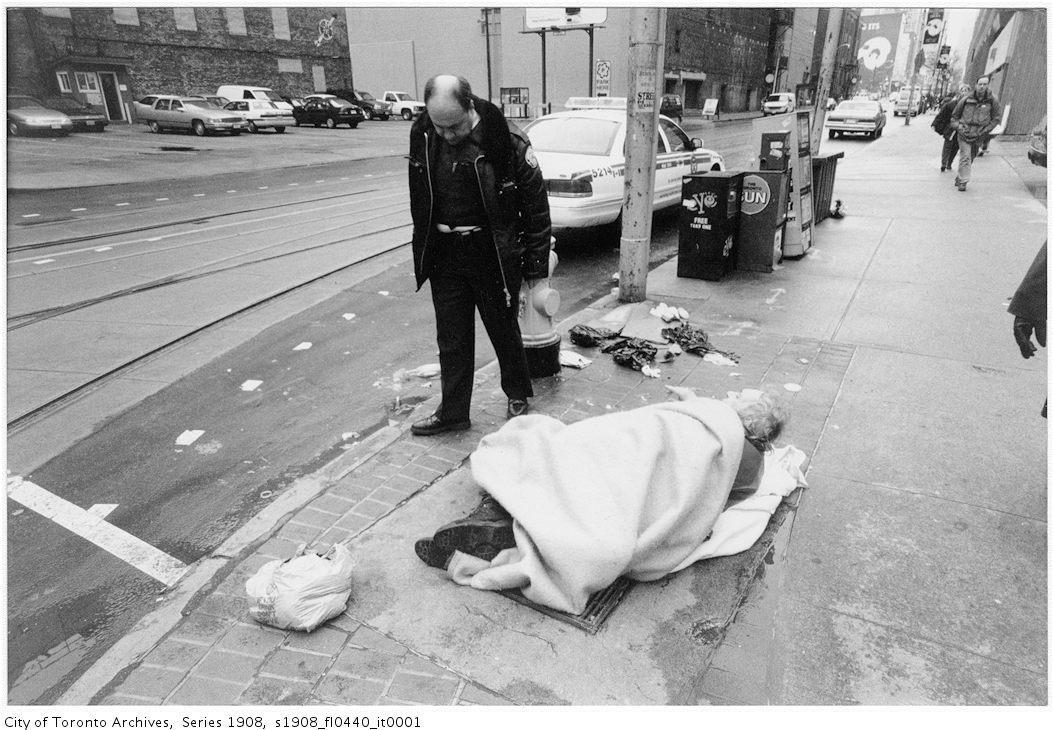
Figure 4.2. This photo depicting police interaction with a community member is from Toronto, but it could be from any large city in America in recent years.
In contrast to the prevalence among the homeless population, about 20% of adults in the general population report having any mental illness, but only 5% report having serious mental illness (such as bipolar disorder or schizophrenia) and 6.7% report having both substance abuse issues and another mental illness (National Alliance on Mental Illness, 2022). Disability is likewise far less common in the overall population than among Portland’s homeless, with about one quarter of all Oregonians experiencing any sort of broadly-defined disability (Oregon Office on Disability and Health, 2010).
