9.5 Commitments in Criminal Proceedings
In contrast to the purely civil commitments discussed in the preceding section, there are several forms of involuntary treatment that occur in the context of criminal proceedings. These commitments are closely connected to an underlying criminal case, but the commitment is not a sentence or a punishment (though it may be perceived that way).
A person who is facing criminal charges may be committed for treatment:
- where they are incompetent to resolve their criminal charges (either temporarily or permanently), or
- where they are found not responsible for criminal acts due to insanity, or in other phrasing, responsible except for insanity.
Both of these situations pause or end the underlying criminal proceedings and give rise to the proceedings described in this section.
A less common type of commitment occurs after conviction and incarceration, where a person convicted of a sex offense remains dangerous and faces continued confinement and treatment to manage that danger.
9.5.1 Commitment to Restore Competence
State psychiatric hospitals across the country, including those in Oregon, are overflowing with committed patients. These are not patients who have been civilly committed due to danger—a group that, as discussed, is now relatively small. Rather, these are patients who were arrested and brought into the criminal system, and then were committed to the hospital. As discussed in Chapter 6 of this text, this group of patients is in the hospital because they are mentally incompetent to proceed in their criminal cases or “aid and assist” in their defense and they are in the hospital to be restored to competence. In Oregon, this commitment and restoration process takes place pursuant to Or. Rev. Stat. § 161.370, and the commitments are most commonly called “370” commitments.
Oregon is not alone in being overwhelmed with criminally incompetent patients, but it is a good example of the problem. The Oregon State Hospital’s daily average population of “aid and assist” patients has skyrocketed in recent years:
- In 2000, the hospital had a daily average of 74 aid and assist patients (just 9 percent of the total hospital population).
- In 2019, the hospital reported an average daily population of 260 aid and assist patients, now over 40 percent of the hospital’s patients.
- In the spring of 2022, there were over 400 daily aid and assist patients – with waiting lists of people in jail needing to enter the hospital for restoration.
Though patients average fewer days in the hospital now than before, even a faster process cannot keep up with the demand for beds (Oregon Health Authority, 2019). As a result, there is a concern that people too mentally ill to resolve their criminal cases must remain in jail for lengthy periods, awaiting their (also lengthy) hospital commitment to undergo a process that will allow them to return to jail. Jail-based restorations, one potential option that would eliminate the need for hospitalization, is being explored in some jurisdictions but thus far has not been done in Oregon. See Chapter 6 for more information on this option.
Lawsuits have pushed for faster hospital admissions, alleging that it is a violation of civil rights to endlessly delay needed treatment for these patients. The legal cases have pointed out the negative health consequences and the fairness problems of keeping very mentally ill people in jail with no treatment. In Oregon, a federal court order resulting from the lawsuit Oregon Advocacy Center v. Mink (D. Oregon 2002) demanded that the state psychiatric hospital take no more than seven days to admit patients who were unable to aid and assist in their criminal defense. Other states have been similarly directed by courts facing this problem. But over the years, compliance is problematic, hampered by shortages of mental health care professionals and the lack of beds in state hospitals.
And even while federal courts have demanded hospitals prioritize this set of patients, some have noted that other groups are suffering at the expense of this one. Only so many beds are available in a state hospital. Should some of them be reserved for civil commitment patients you have just learned about—those who have committed no criminal offense? And what about patients who have been found guilty except for insanity of serious crimes? Beds must be available to hold patients who have nowhere else to be safely held.
The reasons for the daunting numbers of competence commitments are numerous and complex. Among them: lack of community mental health treatment access for people in need prior to criminal system involvement. Untreated, people with mental disorders are coming into the criminal justice system in large numbers, as described in Chapter 4 of this text. Patients who are not competent to resolve their cases are a portion of that group.
Meanwhile, shortages of mental health professionals create a barrier at all levels of care, including hospitals and alternative community settings. This access issue, even at the higher levels of care, exists in Oregon and other states, slowing patient progress through the system (Kaiser Family Foundation, n.d.; Zhu et al., 2022). In 2022, the Oregon State Hospital’s ongoing struggles with staff shortages required closure of units and reduction of admissions (Salem Reporter, 2022).
Further, despite efforts to move patients through the process quickly, restoration of competence is often a slow process that takes months. For example, there are limits on the treatment that can be provided to advance competence; it may be clear that psychiatric medications (figure 9.10) would benefit a patient, but if those are declined, there are limits on doctors’ ability to administer those involuntarily in order to make a person competent to stand trial. Sell v. United States (2003).

Figure 9.10 is a picture of various forms of medication. Certain medications, including some psychiatric medications, are invasive (such as injectable medications) or have side effects that make them unattractive to patients. Forced administration of medications is an additional imposition on bodily autonomy that is not legal absent certain conditions and procedures.
Fortunately, perhaps, restoration efforts are not endless. In the face of hospital backlogs, Courts have moved towards stricter limits on the time allowed to attempt competency restoration. Under previous rules in Oregon, for example, patients could attempt restoration for years in a hospital setting. In August of 2022, however, a federal court in Oregon set new, much shorter, time allowances for restoration of patients at the Oregon State Hospital. Under these new rules, lower level offenders being restored would have to be released after no more than 90 days, and those who are charged with nonviolent felonies would have to be released in 6 months (Oregon Health Authority, 2022). Though this adjustment might reduce overcrowding at the hospital, the question remained: where would these patients go up on release, and would they (and the community) be adequately served? In Oregon, negotiations and challenges around these limits are ongoing.
9.5.2 Extremely Dangerous and Resistant to Treatment
Some patients, despite attempts at restoration, are found “never able” to aid and assist. That is, they are deemed permanently or indefinitely incompetent to resolve their criminal cases. At this point, prosecutors are generally forced to dismiss charges (at least temporarily) against the person who cannot be made competent to resolve those charges. This can be a terribly unsatisfying solution for the justice system, and certainly for victims. It is a difficult situation for the accused person as well, who is left in a sort of limbo, unable to resolve their case with finality.
The Massachusetts case of Jose Veguilla, introduced in Chapter 6, is just such a case. Mr. Veguilla, his family, and his victim’s brokenhearted loved ones have watched as his case churns in an endless cycle of evaluations and hearings – which will never result in a finding of competence. “[E]very few months, the court convenes to discuss his case. A judge receives the update that Veguilla still has severe dementia and cannot proceed. And they agree to have the same hearing several months later. The hearing in January [2023] lasted less than 60 seconds” (Thompson, 2023, para. 44).
Oregon’s solution to cases like Veguilla’s was a statute, enacted several years ago, providing for the involuntary commitment of people who are deemed Extremely Dangerous and Resistant to Treatment (Or. Rev. Stat. §426.701 & 702). This statute is specifically targeted and used to manage people who have committed a most serious offense (e.g. murder, rape), and who have an entrenched mental disorder that is not amenable or responsive to psychiatric treatment. In practice, this often involves people who were charged with a very violent offense, but who simply cannot be made competent to resolve that charge.
The Oregon law first requires that the person be found “extremely dangerous,” a criteria based on the offense committed and a likelihood of repeated harm. The person must also be “resistant to treatment.” If restoration to competence was attempted and failed, and the person was found never able to proceed to trial – and continues to exhibit those same challenges – that information would indicate resistance to treatment.
If a person meets the qualifications, Oregon law allows commitment to involuntary hospitalization and treatment for two years, with an option for recommitment every two years. If the person stops qualifying for recommitment, and becomes competent to proceed to trial, the prosecutor may re-open the underlying criminal case against the person.
Oregon patients committed under the Extremely Dangerous and Resistant to Treatment statute continue to receive treatment for their underlying mental disorders—and, despite barriers, are sometimes able to move out of the hospital and into less restrictive housing and treatment options. Patients committed under the statute are supervised by the Oregon Psychiatric Security Review Board, discussed in more detail in the next section.
9.5.3 Commitment After Insanity Defense
Competing for bed space at state hospitals are patients who have been committed for treatment after successfully asserting the insanity defense in criminal court. These are patients who have been found not guilty by reason of insanity, or, in Oregon, guilty except for insanity (GEI). As you have learned, a successful insanity defense excuses a person from criminal responsibility for an offense based on the impact of a mental disorder. See Chapter 6 for a detailed discussion of the insanity defense. The excused person is not simply released as they would be with other “not guilty” verdicts; they are ordered into a term of treatment designated by state law. This type of involuntary treatment after a criminal matter is sometimes referred to as a criminal commitment — as distinguished from the civil commitments discussed at the beginning of this chapter, which do not involve criminal charges.
Most people who are excused from criminal responsibility due to insanity are committed to a public psychiatric hospital (such as the Oregon State Hospital) for treatment and to ensure community safety (figure 9.11). The details of hospital treatment programs are beyond the scope of this text, but there are many opportunities and therapies available for different types of patients at the Oregon State Hospital. Programs will differ by state. Feel free to learn more about the programs at the Oregon State Hospital [Website].

Figure 9.11 is a photo taken in 2011, showing the western facade of the modern Oregon State Hospital.
Legal oversight of a person’s criminal commitment is generally managed by some combination of medical providers and legal personnel in the criminal justice system. In the federal system, for example, the person is supervised by a U.S. Probation officer, sometimes for life. A few states, including Oregon, have specialized systems to supervise people under criminal commitments. Oregon’s Psychiatric Security Review Board, or PSRB, is a somewhat unique oversight board that is composed of professionals from multiple relevant disciplines. Oregon’s PSRB is charged with ensuring proper management and community safety with respect to all GEI patients, as well as Extremely Dangerous and Resistant to Treatment patients discussed in the previous section. Board members include a psychiatrist, a psychologist, a criminal lawyer, a parole and probation officer, and a community member – each bringing different expertise and perspective to their supervision duties.
In order to perform its duties, the PSRB holds public hearings where the supervised person is in attendance, represented by an attorney. The state, interested in public safety, is also represented by an attorney at PSRB hearings. Hearings may involve testimony from witnesses – primarily treatment providers – who will advise the Board of the person’s mental health status and progress in treatment. Sometimes, hearings are an opportunity for the person and their treatment providers to request that a person be allowed conditional release from the hospital, meaning that the person is permitted to live in the community, often in a group setting, to participate in treatment under a set of rules and safeguards. If those conditions of release are violated, the person may be returned to the hospital. If you are interested, you may read more about Oregon’s PSRB here [Website].
Typically, people who have been criminally committed after an insanity verdict are ordered to remain under the supervision provided in their state for either an indefinite period or for the maximum length of time allowed by their underlying offense. However, if at some point it is determined that the person no longer meets criteria for a criminal commitment – they no longer have a qualifying mental disorder or it no longer makes them dangerous to others – then the person must be released from supervision. Again, the standards for continued commitment and supervision in these circumstances will vary according to the law of the jurisdiction. However, note that the criminal commitment standard is different from that used to civilly commit a person as discussed earlier in this chapter. Civil commitment can be based on a person’s danger to themselves. A criminal commitment typically requires that a person be dangerous in a serious way to other people.
Regardless of how patients are managed or supervised in a particular state, their treatment can be a source of stress and concern to crime victims (figure 9.12) who may feel that justice was not served when the person with a mental disorder was “excused” from responsibility (Lyons, 2007). There can also be an understandable sense of resentment against patients who are able to access mental health care after committing serious offenses, when people who have not found their way into the criminal system can be very limited in their access to mental health care.
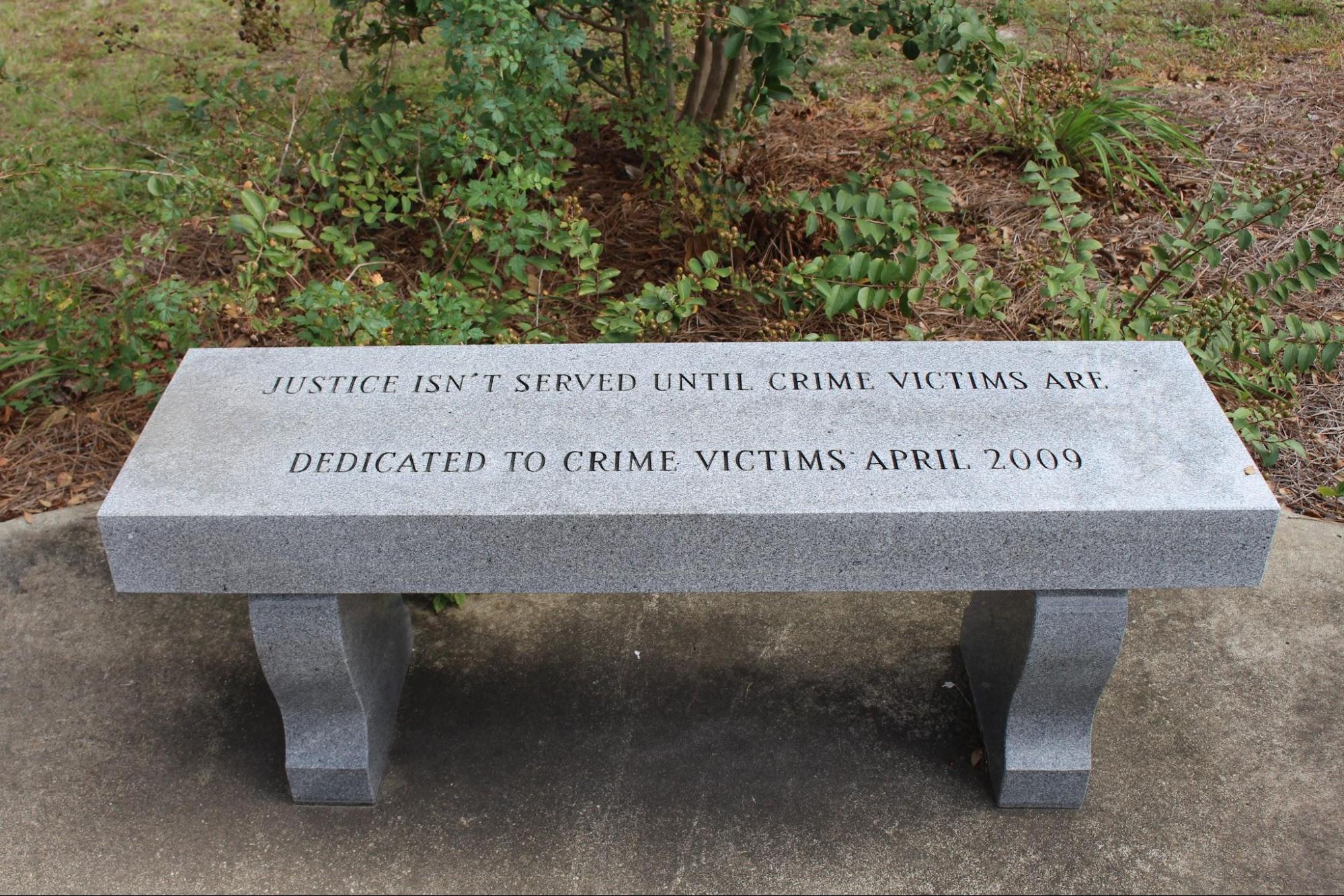
Figure 9.12 shows a picture of a bench, carved with a dedication to crime victims, reading: Justice isn’t served until crime victims are. This sentiment reflects an ongoing concern in all criminal justice proceedings that victims are not always well-served, or supported and cared for, by the criminal justice process. This may feel especially true where offenders are not convicted due to mental disorders.
9.5.4 SPOTLIGHT: The Criminal Commitment Of Andrea Yates
When a person with a serious mental disorder commits a terrible act that they certainly would not have done had they been well, the tragedy seems magnified, and the story of Andrea Yates fits that category. Yates’ story is a difficult one to read and absorb. It is an example of an act that would be a terrible crime, except for the presence of mental illness in the offender. Is this a case where you believe the insanity defense was appropriately applied? Was commitment to a hospital the right outcome in this case?
Andrea Yates (figure 9.13) began as a happy young wife. She and her husband wed in April of 1993 and soon announced that they planned to have as many children as they could during Andrea’s reproductive years. It was after the birth of their fourth child that Andrea first showed signs of severe mental illness.
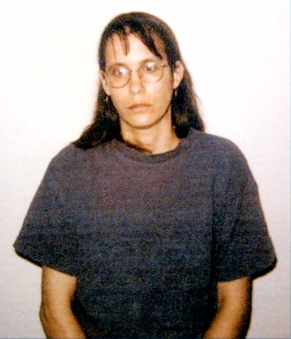
Figure 9.13. Andrea Yates is shown in a Houston Police Department photo in 2001, after the killing of her children.
On June 16th of 1999, Russell Yates found his wife shaking and chewing her fingers. She attempted suicide the following day and was prescribed antidepressants. Just weeks later, she again held a knife to her own throat and begged her husband to let her die. After this second suicide attempt, Andrea was hospitalized, diagnosed with post-partum psychosis, and prescribed several different medications that included anti-psychotics. Andrea’s psychiatrist urged Andrea and Russell not to have any more children, but she was pregnant with the couple’s fifth child within 2 months of her diagnosis.
In November of 2000, the fifth child was born. Andrea seemed stable for a few months, until her father died in March of 2001. This is when her psychosis returned in full force, leading Andrea to regularly mutilate herself. She became fully immersed in the Bible, her religious beliefs now becoming fixations. Between March and June of that year, she was hospitalized twice. After Andrea’s release in June of 2001, her doctor told Andrea’s husband to monitor Andrea around the clock. Unfortunately there was a 1-hour block of time on the morning of June 20th where Andrea was alone with the five children, during which time Andrea drowned all five of the kids one by one. She then called 911 and her husband.
Andrea suffered from psychotic delusions. In her mind, she believed she was saving her children. She later reported to her prison psychiatrist that she believed her children were not righteous because she, herself, was evil. She believed that their souls could never be saved because of who she was, and killing them while they were young would be their only salvation.
Andrea’s first trial took place in 2002 and resulted in a guilty verdict with a sentence of life imprisonment. It was later discovered that a psychiatrist who had testified for the prosecution gave false testimony during her trial and the conviction was overturned. A second trial in 2006 resulted in a not guilty by reason of insanity verdict. Andrea was committed to a psychiatric hospital where she remains to this day – refusing each year to seek release at her annual hearings.
9.5.5 Commitments in Criminal Proceedings: Licenses and Attributions
“Commitments in Criminal Proceedings” by Anne Nichol is licensed under CC BY 4.0.
“Spotlight: The Criminal Commitment of Andrea Yates” by Monica McKirdy is licensed under CC BY 4.0.
Figure 9.10. Image of medications from Pixabay, CC0, via Wikimedia Commons.
Figure 9.11. Photo of Oregon State Hospital by Josh Partee, CC BY-SA 2.5 <https://creativecommons.org/licenses/by-sa/2.5>, via Wikimedia Commons
Figure 9.12. Image of carved bench by Michael Rivera, CC BY-SA 4.0 <https://creativecommons.org/licenses/by-sa/4.0>, via Wikimedia Commons
Figure 9.13. By Houston Police Department, Texas, U.S. – Andrea Yates: 20 Years After Drowning Her 5 Kids In A Bathtub “To Save Their Souls”, Investigation Discovery – CBS News, dated: 2021, Fair use, https://en.wikipedia.org/w/index.php?curid=69305132
