2.7 Substance Use and Co-Occurring Disorders
Substance use disorders involve the recurrent use of alcohol and/or drugs, causing clinically significant impairment of life functions – including health impairments or failure to meet major responsibilities at work, school, or home. Substance use disorders are commonly found in – and out of – the criminal justice system. According to the National Institute of Mental Health, a substance use disorder (SUD) is a mental disorder that affects a person’s brain and behavior, leading to a person’s inability to control their use of substances such as legal or illegal drugs, alcohol, or medications. Symptoms can range from moderate to severe, with addiction being the most severe form of a substance use disorder (NIMH, 2023).
Certain substances of abuse vary by age, race, and geographical location. Substances of abuse definitely go through trends depending on many factors including drug trafficking rings, unintended consequences of prescription medication distribution, and accessibility of abusable substances. Most recently, fentanyl abuse and overdose deaths have driven harm reduction and overdose prevention efforts.
Occasionally it can be very challenging to determine if particular symptoms are related to substance abuse or to a different mental disorder. Substance use can have a major impact on the brain, which influences behaviors. It is important to understand the impacts that using substances can have on a person’s immediate mental well-being and how long-term use can greatly impact cognitive functioning over time. Research increasingly indicates that certain substances (amphetamines and cannabis, for example) are closely related to development of early psychosis and may exacerbate underlying psychotic disorders, or even cause psychotic symptoms (Hartney, 2023).
Indeed, many people who have substance use disorders also have other mental disorders, whether these are causally related or not. According to the National Institute of Mental Health, about half of individuals who experience a SUD during their lives will also experience a co-occurring mental disorder and vice versa (figure 2.17). A co-occurring disorder is when someone is diagnosed both with a mental disorder and a substance use disorder.
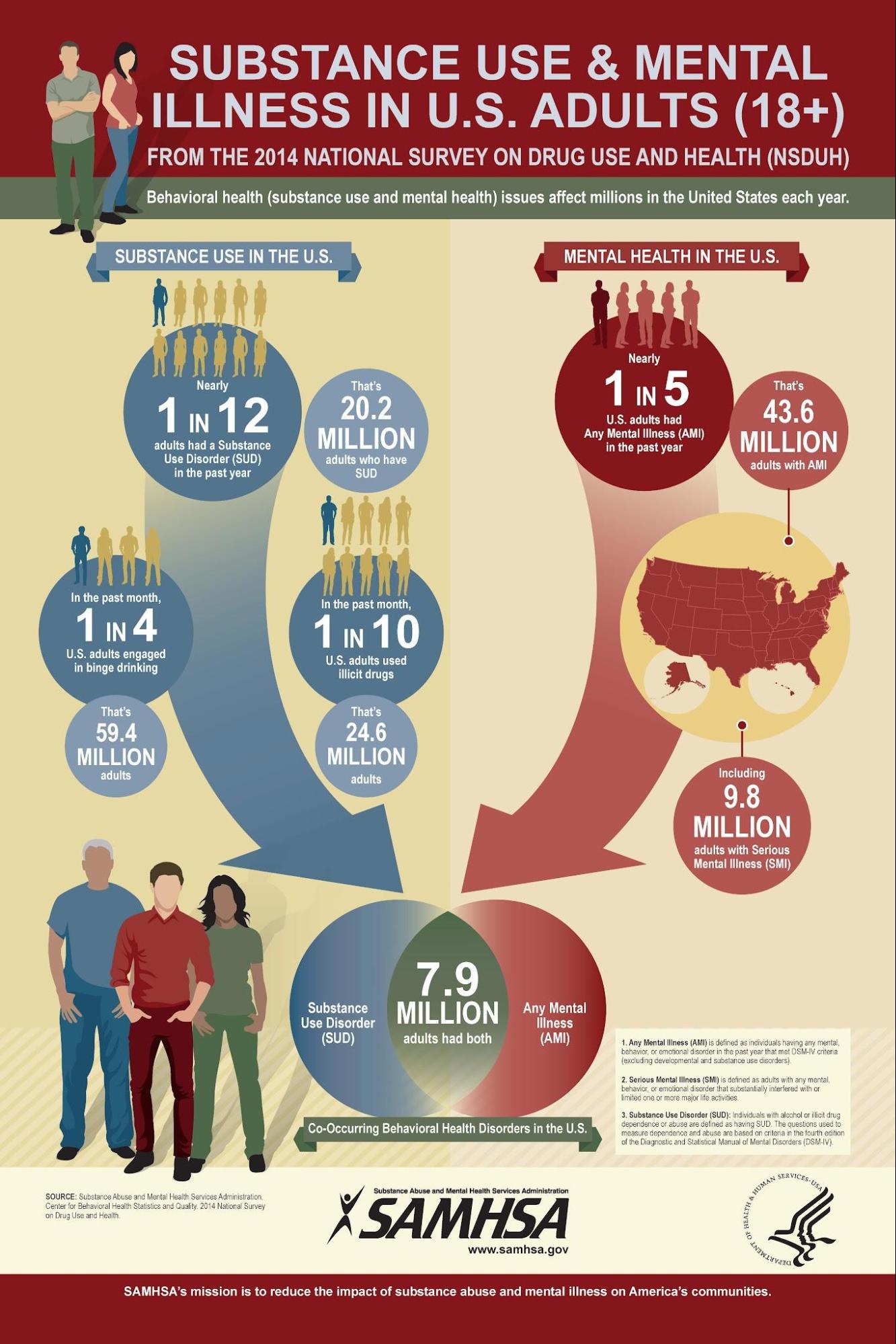
Figure 2.17 provides estimates of numbers of people experiencing substance use disorders and mental health disorders in the United States, with an intersection of nearly 8 million people who experience both, known as co-occurring disorders.
Research suggests three possibilities that could explain why SUDs and other mental disorders may occur together:
- Common risk factors can contribute to both SUDs and other mental disorders. Both SUDs and other mental disorders can run in families, suggesting that certain genes may be a risk factor. Environmental factors, such as stress or trauma, can cause genetic changes that are passed down through generations and may contribute to the development of a mental disorder or a substance use disorder.
- Mental disorders can contribute to substance use and SUDs. Studies found that people with a mental disorder, such as anxiety, depression, or post-traumatic stress disorder (PTSD), may use drugs or alcohol as a form of self-medication. However, although some drugs may temporarily help with some symptoms of mental disorders, they may make the symptoms worse over time. Additionally, brain changes in people with mental disorders may enhance the rewarding effects of substances, making it more likely they will continue to use the substance.
- Substance use and SUDs can contribute to the development of other mental disorders. Substance use may trigger changes in brain structure and function that make a person more likely to develop a mental disorder.
2.7.1 Licenses and Attributions
“Substance Use Disorders” by Kendra Harding is licensed under CC BY 4.0. Adapted from the National Institute of Mental Health website, which is in the public domain.
Figure 2.17. Substance Use in U.S. Adults by SAMHSA is in the public domain.
