9.5 Abortion, Pregnancy, and Childbirth
Worldwide, 140 million babies are born on an annual basis. The U.S. birth rate has been declining since 2007, with only 3.61 million births in 2020. About 8.24% of pregnancies resulted in low-birthweight babies (below 2500 grams or 5.5 pounds), about 10% are born preterm (born alive before 37 weeks gestation), and the mean age at first birth is 27.1 (CDC 2022). What is considered a live birth or fetal death is standardized in medical literature, but reporting of live births and fetal deaths vary by state depending on gestational age and weight.
As discussed in the early part of this chapter, women’s access to quality healthcare means better outcomes for pregnancies and births, which leads to healthier babies and adults. Figure 9.13 shows a pregnant person and their partner. Regulation of pregnancy for some women who have health issues is a life-or-death situation. Women undergoing cancer treatment, who have had or need an organ transplant, certain liver diseases, and other health concerns may need to regulate pregnancy throughout their lives (Linkeviciute et al. 2022; Ahmed et al. 2013: Borgers et al. 2021).
One study of 17 pregnancies in pancreas and kidney transplant recipients found “adverse fetal and graft outcomes were observed in 100% of unplanned pregnancies, compared to 10% of planned pregnancies” (Punjala et al. 2021:1). Debates about access to medications that regulate pregnancy are regularly seen in the media. When politics and religion enter into the discussion of controlling pregnancy, there are serious consequences for women whose health, the success of their pregnancies, or even their life, may depend on access to medications which regulate pregnancy.

Figure 9.13. A pregnant person and their partner. Physical and emotional support of a pregnant person benefits pregnant people and their babies.
9.5.1 Pressure on Female Bodies
Scientifically accurate information about pregnancy and childbirth is not always accessible to everyone. This can lead to ideas that pregnancy and live births resulting in healthy newborns are easy and routine endeavors. “Many of the earliest women’s health books were written by monks, the very people who had the least use for the information” (Epstein 2010).
Women regulating pregnancy has occurred throughout history. Natural remedies such as blocking the vagina with leaves and using plant-based spermicides are found in ancient artifacts (O’Reilly 2021). Fast forward to the 1960s when the birth control pill became widely accessible. During the 1960s, women’s rights activists advocated for changes to laws and societal norms for women’s freedom to control their bodily functions.
Then and today, stereotypes and societal norms maintain that all women would like to be mothers. This is untrue. Not all women want to or are biologically able to become pregnant, carry a pregnancy to term, or can care for a child. Doctors may push back against women’s requests to have their tubes tied or other forms of permanent pregnancy regulation for women who do not have children.
As discussed in the next chapter on media, society instills and maintains stereotypes and expectations for post-pregnancy body image through the media. Social media covers celebrity images of “bouncing back” or returning to a pre-pregnancy body form soon after birth. The reality is that women’s body shapes change due to pregnancy. An article by the Mayo Clinic on post-pregnancy fitness states that in pregnancy, women “gain 25 to 35 pounds, much of it in the span of just a few months. The uterus and its lining will enlarge 500 times its normal size by the end of pregnancy” (Mayo Clinic N.d.). Other agents of socialization, such as religion, family, work, government, and school, also perpetuate images and stories of women’s destiny to become mothers.
9.5.2 Eugenics Practices
Medical science has relied on the biases, values, and norms of its researchers to provide direction for what areas of medicine should be studied. The perceived inequity between groups has been substantiated by social and medical researchers for centuries. Historically, ideas existed of different groups of people being more or less worthy to exist than others, including differences based on gender, race, intelligence, physical ability, mental ability, and other diversities.
Eugenics is the effort to make the human race “better” by removing people thought to be unintelligent, disabled, or mentally ill. In the eyes of the eugenics proponents, these people were considered less beneficial to the human race than others. This also included people of color and some religious groups. Although ancient societies promoted practices of preferring some groups’ reproduction over others for society’s benefit, the substantiation of eugenics only took root in the mid-1800s. One of the ways the United States implemented eugenics was through forced sterilization. This will be discussed later in this chapter in the section on violence.
9.5.3 Abortion Rights
For centuries, women have controlled pregnancy through various methods. Stories of using berries and herbs by indigenous and colonial populations are found throughout history books. “Early term abortion in the founding days of the country was a morality issue, not a criminal one” (Phillips 2022) one researcher writes. Abortion is defined as the spontaneous or voluntary termination of pregnancy. Infanticide occurred throughout history for a variety of reasons, including lack of access to safe, reliable abortion during pregnancy, lack of awareness of being pregnant, and financial constraints.
During the 1900s, the Victorian era tightened control of women’s healthcare as it became regulated by formalized medicine run by White males. As women and people of color gained the right to vote and control their lives throughout the early to mid-20th century, abortion rights also came to the forefront. On January 22, 1973, the Supreme Court affirmed the right to a woman’s privacy in matters surrounding her pregnancy in a 7-2 decision, commonly known as Roe v. Wade. The decision reads in part:
The Due Process Clause of the Fourteenth Amendment protects against state action the right to privacy, and a woman’s right to choose to have an abortion falls within that right to privacy. A state law that broadly prohibits abortion without respect to the stage of pregnancy or other interests violates that right. Although the state has legitimate interests in protecting the health of pregnant women and the “potentiality of human life,” the relative weight of each of these interests varies over the course of pregnancy, and the law must account for this variability. (Oyez N.d.)
Since then, women have had access to abortion services in all U.S. states. On June 24, 2022, access to abortion was removed as a federally protected right and left to each state to decide the issue. The privacy and rights of the pregnancy itself, the rights of the pregnant person, and the rights of community members, family members, or states to regulate a person’s pregnancy has become a highly complex and messy societal issue.
The Supreme Court’s decision to have states decide abortion rights has negatively impacted other aspects of women’s healthcare. Complicated pregnancies that put the mother’s life at risk or where the baby will not grow to term or survive if delivered have doctors weighing aborting the pregnancy and facing possible legal action by states if they do. In mid-October 2022, a doctor was concerned about legal action in one case where the fetus would not survive at birth. The woman endured “a roughly six-hour ambulance ride to end her pregnancy in North Carolina, where she arrived with dangerously high blood pressure and signs of kidney failure” (Kusisto 2022).
9.5.4 Medicalization of Pregnancy and Birth
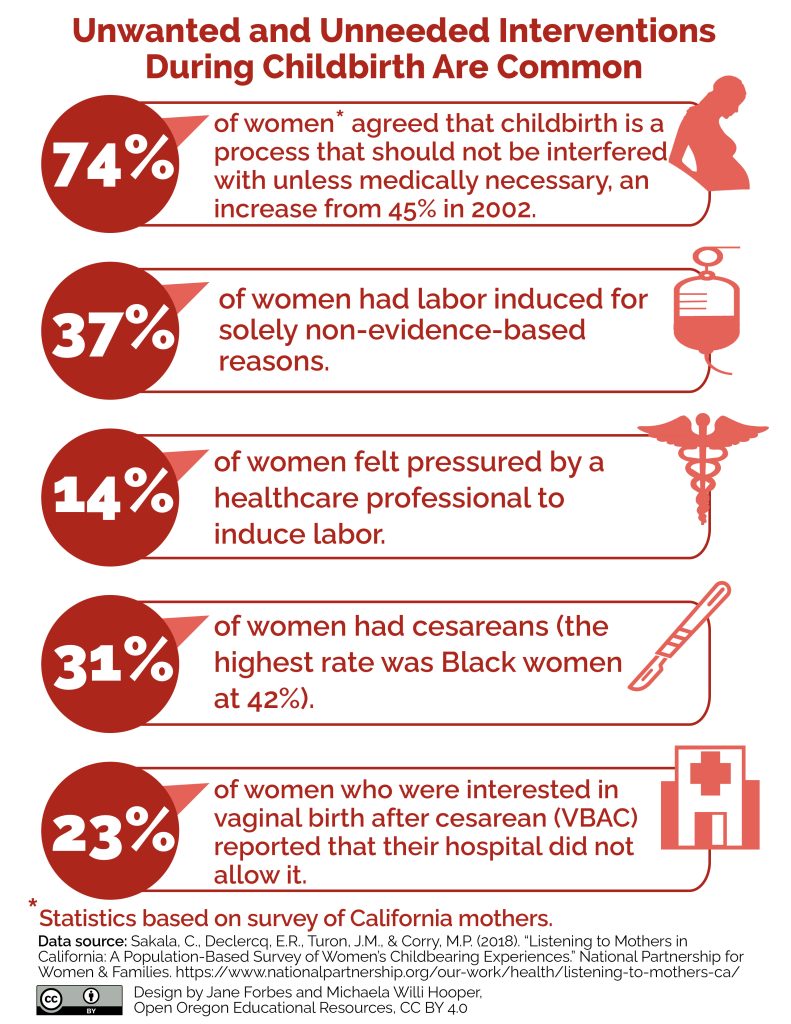 Figure 9.14a. This infographic describes the ways pregnancy and birth have become medicalized, or connected to medical treatment. Figure 9.14a Image Description.
Figure 9.14a. This infographic describes the ways pregnancy and birth have become medicalized, or connected to medical treatment. Figure 9.14a Image Description.
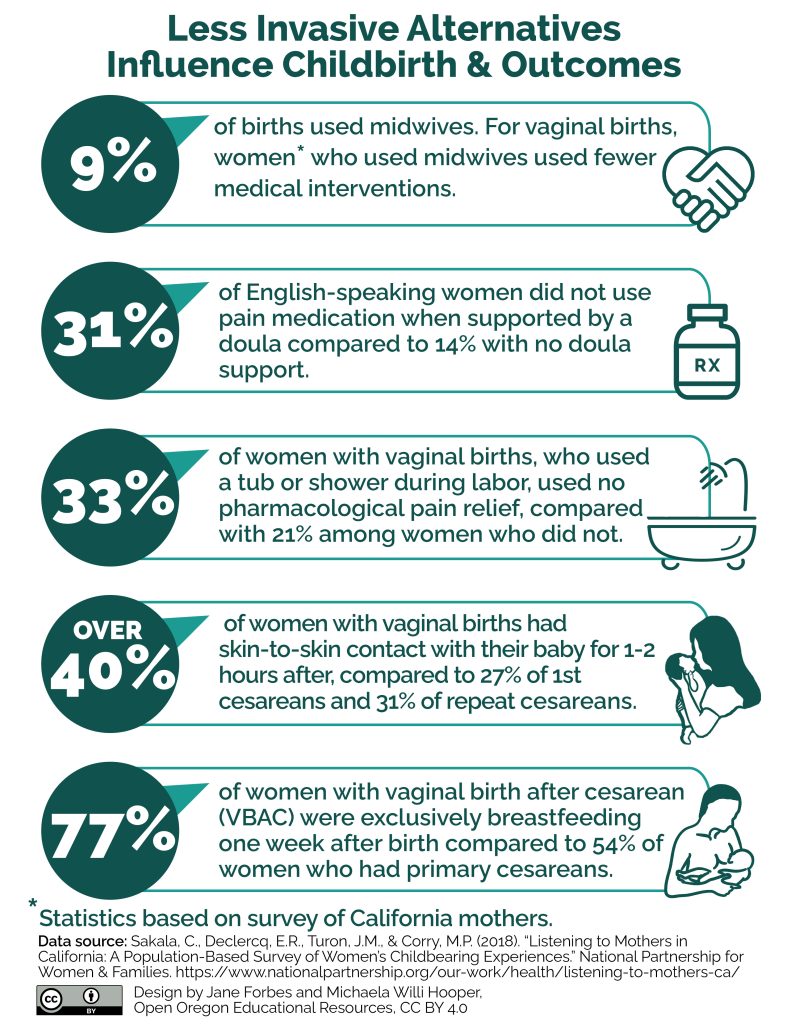 Figure 9.14b. This infographic describes how less invasive alternatives influence childbirth and outcomes. Figure 9.14a Image Description.
Figure 9.14b. This infographic describes how less invasive alternatives influence childbirth and outcomes. Figure 9.14a Image Description.
Changing technology and societal norms over the last 100 years have impacted pregnancy and childbirth, though naturopathic remedies to assist in becoming pregnant and easing childbirth have existed for all time. Childbirth was a female-centric activity with little male involvement. Childbirth regulation within the formal structure of a hospital increased in the last few hundred years, with tools such as anesthesia, forceps, and surgical interventions like cesarean sections becoming a more common practice (Johnson, Newburn Macfarlane 2016).
At the beginning of this chapter we learned about a transgender person’s pregnancy. Transgender and nonbinary pregnancies have been influenced by changing technology as well as societal norms. While gender affirming care from female to male can include hormones and surgery, transgender men may still become pregnant. One study found that “unintended pregnancies occur in up to 30 percent of transgender men” (Brandt et al 2019).
Medical advancements and interventions have remarkably increased survival for both baby and birther. In the United States in the mid-1950s maternal mortality rates sharply declined due to medical research and hygiene practices such as hand washing by medical professionals between patients, antibiotics, and advancement of blood transfusions. The first half of the 19th century, maternal mortality was between 800-1000 deaths for every 100,000 births, dropping to a low of between 6.6-9.2 deaths in the 1980s. Since then, maternal mortality rates have fluctuated yet gradually risen to 23.8 deaths in 2020 and 32.2 deaths per 100,000 births in 2021. (Roser and Ritchie 2013).
Medical guidance for performing cesareans has fluctuated over the years as reflected in changing cesarean delivery rates. In the United States there was a 60% increase in the overall percentage of cesarean deliveries from 1996 to 2009. The rate of cesarean deliveries then declined from 2009 to 2019, “reaching 31.7% in 2019 (2) before increasing in 2020 (31.8%) and 2021 (32.1%) (3)” (Osterman 2022).
Some medical communities today say that many surgical deliveries and childbirth regulations are medically unnecessary. Figure 9.15 shows the cesarean section surgical procedure. A study by Johnson, Newburn, and Macfarlane (2016) reports that “in Spain, obstetric care includes routine enemas, pubic shaving, and episiotomy, procedures that are not evidence based and which ignore the WHO’s guidelines on the care of women in labour”(Johnson, Newburn Macfarlane 2016:892).

Figure 9.15 shows a newly born baby delivered via cesarean section surgery.
9.5.5 Crisis in Black Mortality Rates
Earlier in the chapter, we looked at a global perspective of life expectancy. In this section, we will look at how people of color, specifically Black women, fare when it comes to abortion, pregnancy, and childbirth. Black pregnant women have multiple statuses that negatively impact their health and life course, known as intersectionality. Intersectionality is the inequalities produced by simultaneous and intertwined statuses and how that influences the life course of an individual or group. These statuses compound to the extent that a crisis of care is occurring for them. “In 2020, the maternal mortality rate for non-Hispanic Black women was 55.3 deaths per 100,000 live births, 2.9 times the rate for non-Hispanic White women” (Hoyert 2020). Deaths attributed to maternal mortality are those related to pregnancy and childbirth, including up to six weeks after birth.
An area of marked increased risk of death for Black women compared to White is during the period of six weeks to one year after birth. These deaths “were 3.5 times more likely among Black women than White women. Postpartum cardiomyopathy was the leading overall cause of late maternal deaths, with Black women having a six-times-higher risk than White women” (NIH 2021).
Providers can improve health issues for pregnant Black women. The medical community can help address this crisis by ensuring pregnant people are comfortable with their providers and are listened to when presenting with health concerns. Access to funded healthcare and insurance will make patients more comfortable seeking care. It will also relieve the financial burden of pregnancy, childbirth, and health-related costs.
9.5.6 Circumcision
Circumcising someone is the act of removing part of their genitalia. For females, circumcision removes all or part of the clitoris and sometimes the labia. Female genital modification may also include sewing the remaining skin and vaginal area together, leaving only a small hole for urination and menstruation, known as infibulation (UNFPA 2022). Upon marriage, the woman’s vaginal area is cut open for intercourse. Often, women again need to be cut further open during childbirth, then are typically sewn narrowly after childbirth.
The practice of female circumcision and genital modification, occurring in about 92 countries worldwide, is recognized by the United Nations as Female Genital Mutilation (FGM). The procedures typically occur without anesthesia for nonmedical or cultural reasons. They can cause severe adverse health consequences such as infections, sexual dysfunction, and childbirth complications. This is why the issue is a concern of human rights. “Recent estimates by WHO, UNICEF, UNFPA, The World Bank and the United Nations Population Division reveal that most high-FGM-prevalence countries also have high maternal mortality ratios and high numbers of maternal death” (UNFPA 2022). Figure 9.16 shows the frequency of female mutilation in African countries as of February 2022.
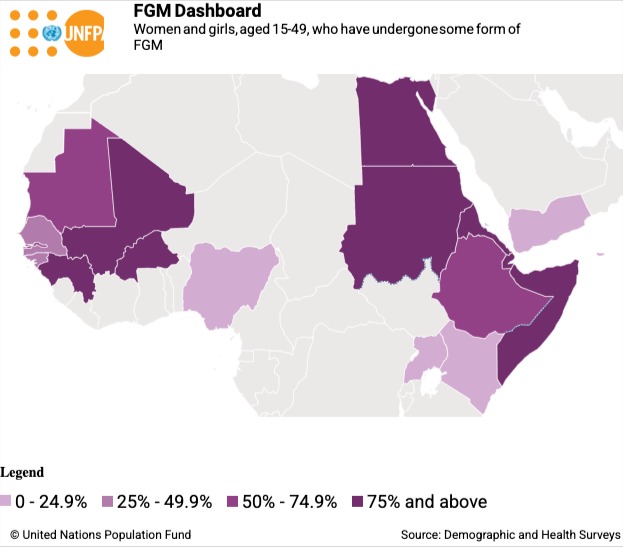
Figure 9.16. Frequency of female circumcision and mutilation by country. From: https://www.unfpa.org/resources/female-genital-mutilation-fgm-frequently-asked-questions#common_types
Why does female genital mutilation occur? Reasons for female genital mutilation, include religion, psychosexual norms prioritizing males’ sexual needs, or the safeguarding of virginity. Also, traditions exist in some cultures such as marital expectations where women are highly dependent on males and coming-of-age cultural traditions (UNFPA 2022).
For males, circumcision removes the foreskin covering the tip of the penis. Approximately one-third of males globally are circumcised. About 80% of adult males in the United States are circumcised (Guevara et al. 2021). Reasons for male circumcision are cultural practices, religious norms, and the father’s circumcision history. There is debate over the procedure’s necessity and health risks or benefits, especially in developed countries such as the United States (Tobian and Gray 2021; Frisch and Earp 2018). Male circumcision is discussed later in this chapter in the section on violence.
9.5.7 Licenses and Attributions for Abortion, Pregnancy, and Childbirth
Intersectionality definition is from the Open Education Sociology Dictionary edited by Kenton Bell, which is licensed under CC BY-SA 4.0.
Figure 9.13. Pregnant person and partner. Photo by Andre Adjahoe on Unsplash.
Figure 9.14a. “Unwanted and Unneeded Interventions During Childbirth Are Common” by Jane Forbes and Michaela Willi Hooper is licensed under CC BY 4.0. Data from Sakala, C., Declercq, E.R., Turon, J.M., & Corry, M.P. (2018). “Listening to Mothers in California: A Population-Based Survey of Women’s Childbearing Experiences.” National Partnership for Women & Families.
Figure 9.14b. “Less Invasive Alternatives Influence Childbirth & Outcomes” by Jane Forbes and Michaela Willi Hooper is licensed under CC BY 4.0. Data from Sakala, C., Declercq, E.R., Turon, J.M., & Corry, M.P. (2018). “Listening to Mothers in California: A Population-Based Survey of Women’s Childbearing Experiences.” National Partnership for Women & Families.
Figure 9.15. Cesarean section. Photo by Jonathan Borba on Unsplash
Figure 9.16. Screenshot of “Women and girls, aged 15-49, who have undergone some form of FGM” by UNFPA is included under fair use.
“Abotion, Pregnancy, and Childbirth” by Jane Forbes is licensed under CC BY 4.0.
Image Description for Figure 9.14a
Unwanted and Unneeded Interventions During Childbirth Are Common
- 74% of women agreed that childbirth is a process that should not be interfered with unless medically necessary, an increase from 45% in 2002.
- 37% of women had labor induced for solely non-evidence-based reasons.
- 14% of women felt pressured by a healthcare professional to induce labor.
- 31% of women had cesareans (the highest rate was Black women at 42%).
- 23% of women who were interested in vaginal birth after cesarean (VBAC) reported that their hospital did not allow it.
Statistics based on survey of California mothers.
[Return to Figure 9.14a]
Image Description for Figure 9.14b
Less Invasive Alternatives Influence Childbirth & Outcomes
- 9% of births used midwives. For vaginal births, women* who used midwives used fewer medical interventions.
- 31% of English-speaking women did not use pain medication when supported by a doula compared to 14% with no doula support.
- 33% of women with vaginal births, who used a tub or shower during labor, used no pharmacological pain relief, compared with 21% among women who did not.
- Over 40% of women with vaginal births had skin-to-skin contact with their baby for 1-2 hours after, compared to 27% of 1st cesareans and 31% of repeat cesareans.
- 77% of women with vaginal birth after cesarean (VBAC) were exclusively breastfeeding one week after birth compared to 54% of women who had primary cesareans.
Statistics based on survey of California mothers.
[Return to Figure 9.14b]

