Lesson 1: Functions of the Integumentary System
Functions of the Integumentary System
By the end of this lesson, students will be able to:
- Explain the functions of the integumentary system.
- Identify the principal structures and layers of human skin.
- Identify Accessory Structures and their function.
Introduction
The integumentary system is a vital and complex organ system that serves as the body’s primary interface with the external environment. In this lesson, we will explore the structure and function of the integumentary system. Our primary objectives are to explain its key functions, identify the principal structures and layers of human skin, and describe the structure and function of accessory structures found in and on human skin.
Functions of the Integumentary System
The integumentary system acts first and foremost as a protective shield, guarding the body from mechanical, chemical, microbial, thermal, and ultraviolet (UV) damage. It also prevents desiccation, plays roles in excretion and vitamin D synthesis, and helps regulate body temperature. See Figure 1.
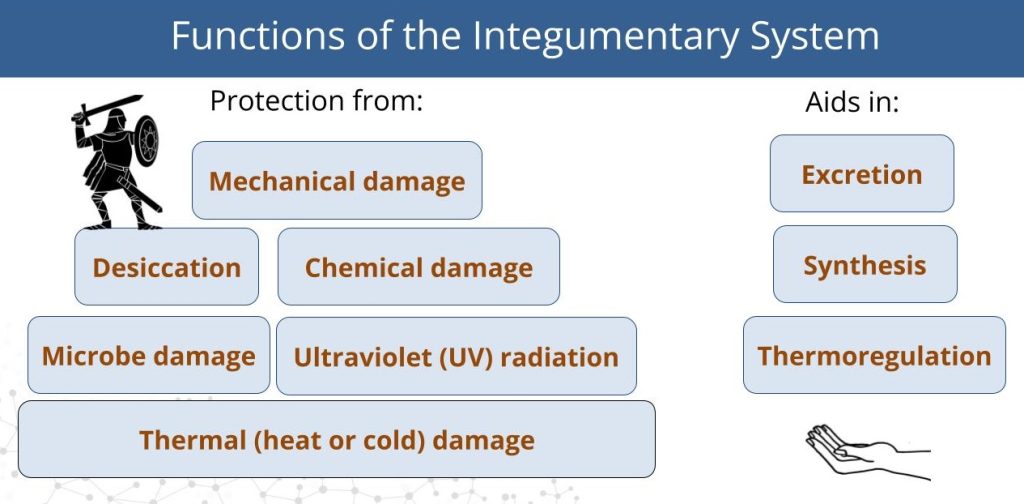
Protection from External Damage
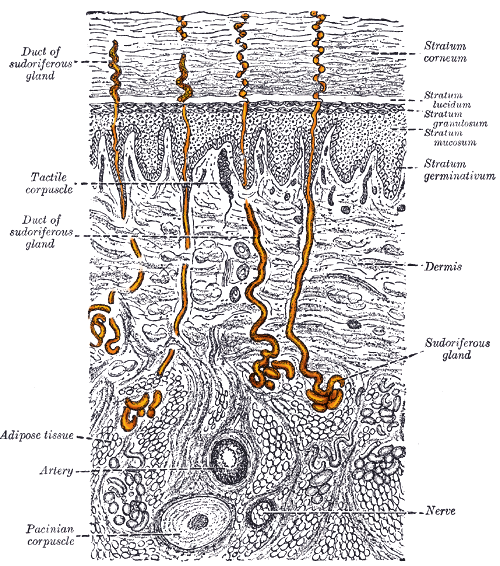
Mechanical Protection: The skin is composed of tough, tightly bound cells rich in keratin—a protein that reinforces the skin’s structure. Beneath the skin lies a layer of adipose tissue that cushions mechanical blows. Sensory receptors embedded in the skin detect pressure and pain, alerting the nervous system to potential injury. See Figure 2.
Chemical Protection: The outermost keratinized layer of skin is relatively impermeable to many aqueous solutions, including acids and bases. The outermost layer of cells are packed tightly, and contain a specialized arrangement of lipids and cells that prevent excessive water loss and entry. See Figure 3. Pain receptors help detect chemical threats, prompting quick behavioral responses.

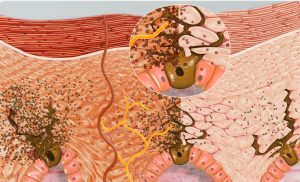
Microbial Protection: The skin serves as a physical barrier against pathogens. Its secretions create an acidic environment (acid mantle) that inhibits microbial growth. If pathogens do breach the surface, immune cells located just beneath the skin can phagocytize and destroy them. See Figure 4.
UV Radiation Protection: Specialized cells called melanocytes, located in deeper layers of the skin, produce melanin. Melanin is a dark pigment that absorbs UV rays, shielding underlying cells from DNA damage. See Figure 5.
Thermal Protection: Heat, cold, and pain receptors help detect environmental temperature extremes, prompting protective behaviors. The skin also contributes to thermoregulation by controlling blood flow through capillary networks near its surface. See Figure 6.
Prevention of Desiccation: The keratinized outer layer contains glycolipids that repel water, preventing dehydration by keeping internal moisture in and external moisture out.
Additional Functions
Excretion
The skin helps eliminate nitrogenous wastes such as urea and uric acid through the sweat glands. Though the kidneys are the primary organ of excretion, the integumentary system contributes by secreting waste in sweat. See Figure 7.
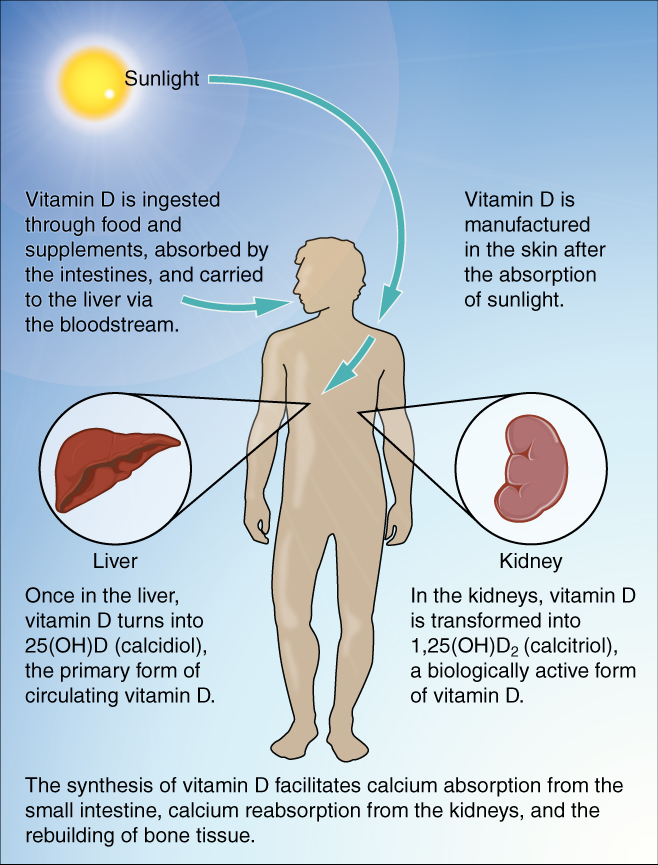
Synthesis of Vitamin D
When exposed to UV rays, cholesterol molecules in the skin are converted into vitamin D. This vitamin is essential for calcium absorption and overall metabolic function, making the skin an important site of chemical synthesis.
Thermoregulation
The integumentary system helps maintain stable internal temperature. When the body overheats, blood vessels in the dermis dilate, allowing warm blood to reach the skin surface where heat can dissipate. This causes the skin to appear flushed or red. Conversely, in cold conditions, blood vessels constrict, reducing blood flow near the surface and preserving body heat—resulting in paler or bluish skin.
Structure of the Skin
The skin has two primary layers: the epidermis and the dermis, with a third supportive layer beneath called the hypodermis. The epidermis is made of closely packed epithelial cells. The dermis is made of dense, irregular connective tissue that houses blood vessels, hair follicles, sweat glands, and other structures. Beneath the dermis lies the hypodermis, which is composed mainly of loose connective and fatty tissues. See Figure 10.
Epidermis
The epidermis is the outermost layer, composed of stratified squamous epithelium. It contains keratinocytes, which produce keratin and form a waterproof barrier. These cells originate in the deepest layer and move upward as they mature, eventually dying and being sloughed off.
The layers of the epidermis, from deepest to most superficial, are:
-
Stratum basale: Contains basal cells that continually divide to produce new keratinocytes.
-
Stratum spinosum: Cells are interconnected by desmosomes, which give the layer a spiny appearance.
-
Stratum granulosum: Cells accumulate keratin granules, preparing for their eventual death.
-
Stratum lucidum (found only in thick skin): A thin, translucent layer present in the palms and soles.
-
Stratum corneum: The outermost layer composed of dead, flattened, keratin-filled cells that are regularly shed.
Other important epidermal cells include:
-
Merkel cells: Sensory cells that detect touch.
-
Langerhans cells: Immune cells that ingest foreign microbes.
-
Melanocytes: Pigment-producing cells that help block UV radiation.
Dermis
Beneath the epidermis lies the dermis, made of connective tissue rich in collagen and elastin fibers. It contains blood vessels, nerve endings, glands, and hair follicles. See Figure 12.
The dermis has two layers with a rich sensory and vascular network:
-
Papillary layer: The superficial region composed of dermal papillae—finger-like projections that increase surface area and strengthen attachment to the epidermis.
-
Reticular layer: The deeper region composed of dense irregular connective tissue that provides strength and flexibility. It houses most of the skin’s accessory structures.
Hypodermis
The hypodermis, or subcutaneous layer, is not part of the skin. It lies beneath the dermis and contains adipose tissue and connective tissue, providing insulation, energy storage, and cushioning. Below the hypodermis, bone and skeletal muscle are typically found.
Accessory Structures of the Skin
The integumentary system also includes several important accessory structures: hair, nails, and glands.
Hair
Hair is composed of keratinized cells and serves several functions, including thermoregulation, sensory detection, and protection. The visible part that extends above the skin is the shaft, while the root is the base anchored in the skin, and the matrix is the region of active cell division that produces the hair. The arrector pili muscle is the smooth muscle attached to the hair follicle that contracts to raise the hair shaft, causing goosebumps. See Figure 13.
The functions of hair include:
-
Sensory reception
-
Protection from UV radiation
-
Thermoregulation (via arrector pili muscle contraction)
Nails
Nails are also made of keratinized cells and provide protection to the fingertips and aid in grasping small objects. The nail body lies on top of the nail bed, and the cuticle protects the growth area at the base of the nail. See Figure 14.
Glands
There are two primary types of sweat glands and one type of oil gland:
-
Sebaceous glands: Produce sebum, a fatty substance that lubricates and waterproofs the skin and hair.
-
Eccrine sweat glands: Widely distributed; produce watery, odorless sweat that evaporates to cool the body.
-
Apocrine sweat glands: Found in the armpits and genital regions, they secrete a thicker, milky sweat that contributes to body odor and may have once played a role in pheromone-based communication.
Both eccrine and apocrine glands contribute to the excretion of metabolic waste such as urea. See Figure 15.
Summary
In this lesson, we explored the essential components and functions of the integumentary system. We discussed its role in protection, excretion, thermoregulation, and vitamin synthesis. We examined the structural layers of the skin, including the epidermis, dermis, and hypodermis, and learned about accessory structures such as hair, nails, and glands. This system is both the body’s first line of defense and a key regulator of internal balance and homeostasis.
Watch this lesson video, walking you through the Module 2 Lesson 1 Integumentary Structure & Function slides.
Practice Questions
Use these practice questions to assess your knowledge before you move on to the next section.

