Lesson 2: Growth,Repair, and Disorders of the Integumentary System
Growth, Repair, and Disorders of the Integumentary System
By the end of this lesson, students will be able to:
- Describe the process of skin repair and the phases of wound healing.
- Relate breakdowns in homeostasis to pathological presentations of the integumentary system.
Introduction
The skin is a dynamic organ constantly renewing and repairing itself—a balance essential for maintaining homeostasis. This lesson explores the normal growth cycle of the skin, the four phases of wound healing, and several common disorders and injuries—from acne and eczema to skin cancer and burns.
Normal Growth and Renewal of Skin
Recall that in thin skin, the epidermis consists of four major layers of cells that are continually renewing:
Stratum basale — Stem cells rapidly divide to supply new keratinocytes.
Stratum spinosum — Daughter cells move outward, forming desmosomal connections.
Stratum granulosum — Cells accumulate keratin-filled vesicles as they mature.
Stratum corneum — Cells die, merging into a keratin barrier that sheds regularly.
As basal cell proliferation matches surface loss, the epidermis maintains a steady thickness. Damage triggers an accelerated, wound-repair response.
Skin Repair: Regeneration vs. Fibrosis
-
Regeneration: Damaged skin is replaced by identical cell types, restoring basic function.
-
Fibrosis: If tissue structure is altered, repair involves scar tissue formation (excess collagen) in the dermis. Over months to years, scars remodel—flattening and fading with improved function.
Phases of Wound Healing
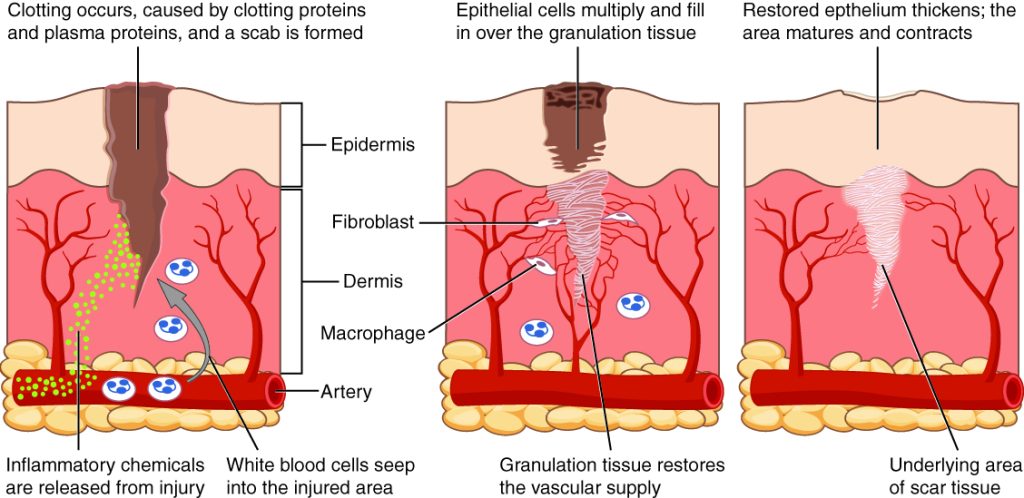
Deep wounds—those involving both epidermis and dermis—progress through four overlapping stages: hemostasis, inflammation, proliferation, and remodeling. See Figure 1.
Hemostasis
-
Damaged vessels expose collagen, triggering platelet aggregation and clot formation via positive feedback.
-
Clots prevent blood loss and block pathogens. Macrophages begin clearing debris under the scab.
Inflammation
-
Mast cells release histamine, increasing capillary permeability.
-
Plasma proteins, antibodies, and white blood cells (neutrophils, lymphocytes) enter tissue via diapedesis.
-
This response produces swelling, redness, heat, and pain—classic inflammatory signs.
Proliferation
-
Granulation tissue forms: new capillaries (angiogenesis) + collagen laid down by fibroblasts.
-
Epithelium regrows through keratinocyte migration and division, closing the wound.
Remodeling
-
The epithelium restores all four normal layers.
-
The dermal scar undergoes gradual remodeling: collagen is reduced and restructured, restoring flexibility and strength over months to years.
Common Integumentary Disorders
Acne
-
Plugged hair follicles accumulate excess sebum and keratinocytes, which encourages Cutibacterium acnes colonization.
-
Inflammation follows: red, swollen pustules and nodules, often driven by androgen-stimulated sebum production.
Eczema
-
Chronic epidermal inflammation, edema, and spongiosis in the stratum spinosum.
-
This leads to the thickened epidermis and keratin build-up, with vesicles and deep dermal inflammation, resulting in itchy, red, raised patches.
Skin Cancers
Uncontrolled proliferation due to UV-induced DNA mutations:
Basal-cell carcinoma — Arises in stratum basale; most common but least dangerous.
Squamous-cell carcinoma — Originates in squamous keratinocytes; treatable if caught early.
Malignant melanoma — Develops in melanocytes; rare but deadly.
ABCDE Warning Signs for moles:
-
Asymmetry
-
Border irregularity
-
Color variation
-
Diameter > 6 mm
-
Evolving shape or pigmentation
Burns and Degrees of Injury
Thermal, chemical, electrical, or UV damage leads to:
-
Protein denaturation and cell death.
-
Systemic impacts—inflammation, fluid loss, infection risk, electrolyte and immune disruptions.
Burn severity:
-
First-degree: Epidermis only – redness, swelling, pain; self-repairs.
-
Second-degree: Epidermis + superficial dermis – blisters form; painful; usually self-heals but slower.
-
Third-degree: Entire epidermis + dermis destroyed; painless due to nerve loss; requires grafting.
-
Fourth-degree: Involves hypodermis, muscle, bone; high risk; surgical intervention required.
Summary
In this lesson, we covered these key points:
-
Skin’s continuous renewal occurs via its four epidermal layers.
-
The four integrated phases of wound healing are hemostasis, inflammation, proliferation, and remodeling.
-
Common integumentary disorders—acne, eczema, skin cancers—and their disruption of homeostasis.
-
Burn types and systemic consequences.
Understanding these processes highlights the complexity of the integumentary system and its vital role in protection, regeneration, and balance.
Watch this lesson video, walking you through the Module 2 Lesson 2 Integumentary Growth, Repair, and Disorders slides.
Practice Questions
Use these practice questions to assess your knowledge before you move on to the next section.

