2.9 Substance Use and Co-Occurring Disorders
Substance use disorders are mental disorders that involve recurrent use of alcohol and/or drugs, despite significant impairment or problems—including health, home, or work problems—caused by the substance use. The use of substances does not constitute a disorder. Rather, diagnosis depends on problems associated with the use: physical dependence on the substance, risky substance use, social problems related to substance use, and/or impaired control related to use (Hartney, 2023a). Symptoms can range from moderate to severe, with addiction being the most severe form of substance use disorder.
The DSM-5-TR recognizes substance use disorders related to ten different classes of drugs, including alcohol, caffeine, opioids, and inhalants (Hartney, 2023a). The substances that are abused in our communities vary by the demographics of users as well as by influencing factors, such as popularity and accessibility of various substances, as well as enforcement and support efforts. Most recently, for example, fentanyl (a powerful synthetic opioid) has become widely abused. Fentanyl overdose deaths have wreaked havoc in many locations. Attempts to address this problem have driven harm reduction and overdose prevention efforts aimed at this specific issue (National Institute on Drug Abuse, 2021).
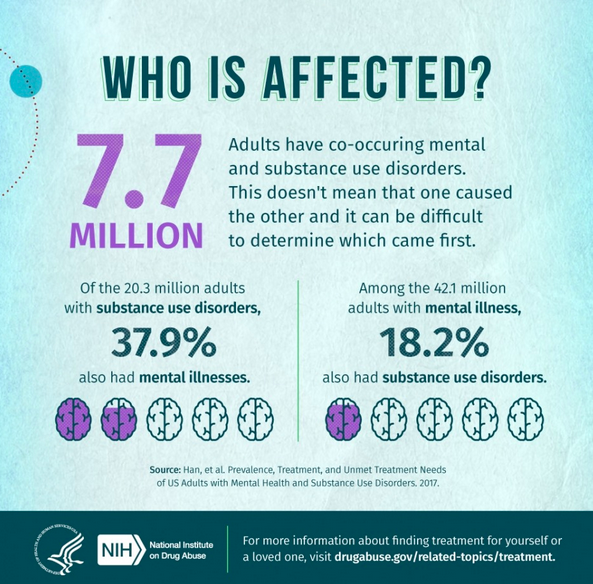
It is common for people with substance use disorders to have other diagnoses as well (figure 2.21). A co-occurring mental disorder exists where someone is diagnosed with multiple mental disorders of any type (e.g., schizophrenia and a personality disorder), but the term is most frequently used where a person has both a mental disorder and a substance use disorder. The term dual diagnosis was formerly used to describe this common situation (Psychology Today, 2021b).
Research suggests several explanations as to why substance use disorders and other mental disorders so frequently occur together. There are common risk factors: both can run in families, for example, suggesting genetic roots. Environmental factors like stress or trauma may contribute to the development of a mental disorder or a substance use disorder. Additionally, people with mental disorders may use drugs or alcohol as a form of self-medication. Finally, substance use can contribute to the development of other mental disorders by triggering changes in brain structure and function that make a person more likely to develop another mental disorder.
Occasionally, these connections and interactions between substance use, mental health, and disability can make it very challenging to determine if particular symptoms are attributable to substance use or a different mental disorder, and, if both are present, which came first. Research increasingly indicates that certain substances (amphetamines and cannabis, for example) are closely related to the development of early psychosis and may exacerbate underlying psychotic disorders or even cause psychotic symptoms (Hartney, 2023b). The DSM clearly recognizes that certain disorders can be attributed directly to substance use with diagnoses such as substance-induced psychotic disorder and substance-induced neurocognitive disorders. The correct diagnosis can have important implications for treatment, as well as for criminal justice proceedings where the cause of a person’s behavior often determines legal outcomes.
Medications have emerged as a very effective treatment for substance use disorders; these medication-based approaches are discussed more in Chapter 8. A number of behavioral therapies are also helpful in treating individuals with substance use disorders, as well as co-occurring disorders. Cognitive behavioral therapy, which was discussed earlier in this chapter, is an effective treatment, as is dialectical behavior therapy (DBT) (figure 2.22). DBT uses concepts of mindfulness and acceptance—encouraging a person to be aware of and attentive to their current situation and emotional state—and other coping skills that help participants manage intense emotions, reduce self-destructive behaviors, and improve relationships. DBT can also be useful in treating several of the other mental disorders described in this chapter.

Licenses and Attributions for Substance Use and Co-Occurring Disorders
Open Content, Previously Shared
“Substance Use and Co-Occurring Disorders” is adapted from the National Institute of Mental Health, which is in the public domain. Modifications by Anne Nichol, licensed under CC BY-NC 4.0, include rewording and expanding upon the content.
Figure 2.21. “Who is affected” is adapted from Comorbidity: Substance Use and Other Mental Disorders by The National Institute on Drug Abuse is in the public domain. Modifications: cropping image for pedagogical impact.
Figure 2.22. “Dialectical Behavior Therapy Skills” by MissLunaRose12 is licensed under CC BY-SA 4.0.

