1.2 Historical Perspective on Mental Disorders
In our modern world, it is often noted that jails and prisons are the United States’ largest mental health facilities, housing and to some extent treating far more people than civilian psychiatric facilities (Chang, 2018). It is difficult, however, to put exact numbers to this fact. According to U.S. Bureau of Prisons (BOP) reporting from 2016, more than 40 percent of prison and jail occupants have a history of a mental illness (Maruschak et al., 2016). This statistic was gleaned by asking jail and prison occupants if they had been informed of their mental illness by a mental health professional – thus failing to count a presumably significant number of occupants who never had access to mental health professionals (due to racial or economic barriers, for instance) or, for reasons that are easy to imagine, did not answer that jailhouse question truthfully.
According to the same BOP study, about a quarter of all prisoners reported having “cognitive disabilities.” Cognitive disabilities would include mental disorders that impact the ability to think, problem-solve, and pay attention. About 25% of prisoners also reported having been in “special education” classes in school, which means that they were identified in childhood as having a disability that impacts learning (Maruschak et al., 2021). Again, these self-reported numbers may not be accurate for various reasons.
In this text, the term mental disorders is used throughout to include both those who experience mental illness and those who have diagnoses such as intellectual disability or a developmental disorder (autism or attention deficit hyperactivity disorder, usually known as ADHD, for example) that impact their functioning. People with mental disorders filling jails and prisons is an outcome that results in commonly reported, though flawed, statistics such as the BOP’s 40 percent, but it is also just a slice of a much larger and more complex issue: the connection between the criminal justice system generally – from the point of arrest to post-prison community reentry – and people with mental disorders.
The overwhelming number of people with mental disorders in the criminal justice system is a modern development. Jails and prisons historically held a small fraction of their current population. In the past fifty years, those numbers ballooned – including for people with mental disorders (Cullen, 2018). United States society and its predecessors have, through time, been unable to or unwilling to meet the needs of this group – or, often, even properly recognize their humanity. The U.S. criminal justice system is the latest inappropriate landing spot for many people with mental disorders, and it is the culmination of the history outlined in this chapter.
1.2.1 Early Treatment of Mental Disorders
Mental disorders have long been met with confusion, denial, fear, and frustration. These reactions have led to poor and misinformed responses and go all the way back to the earliest history of mental disorders. While history is not our primary focus, this text considers the treatment of people with mental disorders over time to see how ignorance and sometimes hostility result in mistreatment. These responses are inextricably woven into our society’s approach to mental disorders.
Prior to the spread of more modern scientific understandings of the brain, mental disorders likely felt especially mysterious and daunting. This led to a common belief in ancient times that mental illness or disability was caused by demonic possession or by an angry god. If someone was “possessed,” treatment would be focused on releasing the “evil spirits” from that person. (Spielman, Jenkins & Lovett, citing Szasz 1960).
The ancient practice of trephination is believed to have been an early way to manage a person who was beset with this kind of problem. Our understanding of trephination is pieced together from archeological finds, including skulls of children and adults where the procedure was performed. Trephined skulls have holes drilled in them, sometimes more than one (figure 1.1). Some researchers believe the holes were intended to allow release of evil or demonic spirits that were causing pain or illness. Scientists believe trephination may have been used to treat seizures or other signs of demonic presence, including mental illness. The procedure may have been done for headaches as well, but one would assume those were very bad headaches! Ancient skulls with trephination holes often show signs of healing where the holes were created, suggesting that many who underwent the surgery survived a least for a time – though it is not known their condition or quality of life post-surgery (Faria, 2013).

Figure 1.1. This trephined skull shows multiple holes that have some evidence of healing, indicating this procedure was not immediately fatal. There is not clear evidence as to why the procedure was done. The pictured skull was recovered in Jericho, part of Palestine now, and is thought to be from around 2000 B.C.
Another ancient treatment option, originating from early Christian beliefs, was exorcism. If a person was experiencing symptoms like delusions or hearing voices, they were seen as possessed by the devil, who was an enemy of god. The devil then needed to be removed, or exorcized, to help the person recover. As shown in figure 1.2, exorcism involved special prayers and rituals conducted by a religious leader (Spielman, Jenkins & Lovett). Unfortunately exorcism has sometimes involved abusive or harmful behavior as well, resulting in injury or even death for people who in all likelihood were experiencing a mental disorder (Thomson, 2021).

Figure 1.2. Pope Pius V performing an exorcism on a woman.
Though the idea of exorcism dates back to new testament accounts of Jesus himself expelling demons from the afflicted, this ritual still lurks on the edges of church practices today. In 1999, the Catholic church issued guidelines on how to conduct an exorcism in modern times (Stammer, 1999). The church did attempt to make clear, when it created the new rules, that the practice should not be viewed as a cure for mental illness. An exorcist is supposed to consider whether a person needs psychiatric help, and perhaps “collaborate” with mental health professionals (Religion News Service, 1999).
Amidst the stubbornly problematic practices, there were also reformers and voices of wisdom around mental disorders, even in ancient history. As early as 500 B.C., Greek physician Hippocrates had begun to treat mental illness as a disease, rather than as a punishment from the gods. Muslim Arabs had created asylums for those with mental illness by the early middle ages (Tracy, 2019). Asylums were places intended as a refuge for confinement and care of those with mental disorders, and later emerged in Europe and America as precursors to mental hospitals and psychiatric facilities. (Ferreras) Religious influences on the management of mental disorders remained powerful over time, up until much closer to the modern day.
1.2.2 Mental Disorders in the Middle Ages & Early Modern Era
In the later middle ages, around the 11th century, the influence of the Roman Catholic church in Europe had grown very powerful. Natural disasters, such as famines and plague, that occurred during this time were thought to be caused by the “devil.” Accordingly, during this same period, religious and spiritual explanations for more individual problems, such as mental disorders, increased in popularity. Treatments for mental disorders tended toward prayers, confessions, and atonement – or asking for God’s forgiveness. (Farreras)
Beginning around the 13th century in Europe, religious leaders began spreading the word that certain people, mostly women, often marginalized ones such as widows, were “witches” (history.com, 2020). Witches were believed to have formed a pact with Satan himself, rejecting Jesus and the church and posing a threat to those around them (Russell et al., 2022). So-called “witch hunts” during the next several hundred years, culminating in the 15th to 17th centuries, resulted in more than 100,000 people being burned at the stake. (Schoeneman, 1977; Zilboorg & Henry, 1941, cited in Farreras) Modern historians are not in complete agreement, but many have concluded that at least some of these supposed witches who were prosecuted and so terribly punished were, in fact, people suffering from some type of mental disorder. Even during the time of the witch hunts, some scholars attempted to argue that the supposed witches were actually mentally ill women, not women possessed by the devil. However, the Catholic church effectively silenced this wisdom by banning their writings. (Farreras)
Meanwhile, beginning in the 1600s, as Europe was emerging from the middle ages, a first step towards the modern era of treating mental disorders began with the growth of institutions, often known as asylums. These early institutions were purportedly intended to shelter mentally ill people, along with other groups such as poor, homeless and disabled people. The real purpose of asylums was to effectively remove undesirable populations from view – protecting the public from asylum occupants – rather than actually helping patients. (Farreras) The conditions inside these early asylums were horrible (figure 1.3).

Figure 1.3. This painting by Francisco Goya, called The Madhouse, depicts a mental asylum and its inhabitants in the early 1800s. The patients are largely naked and appear to be in a dungeon setting.
Two infamous institutions operating in the 1700s and beyond were “Bedlam” hospital in London (properly named St. Mary of Bethlehem) (figure 1.4) and La Salpêtrière, an asylum for women located in Paris that held thousands of patients (figure 1.5). Both of these institutions were essentially dungeons; mentally ill patients were often chained to walls alongside other unfortunate occupants – the sick and the poor (Tracy, 2019). Asylum patients throughout Europe were sometimes displayed to the public, or exhibited, for a fee. (Farreras) It is telling of the scene in these asylums that London’s Bethlehem hospital was casually called “Bedlam,” and that this name was the origin of the modern term “bedlam,” meaning a wild and chaotic situation (Merriam-Webster, n.d.).

Figure 1.4 – William Hogarth’s Scene from Bedlam, created in 1734, shows the chaotic situation in London’s Bedlam hospital, with a man in chains surrounded by others engaged in various unusual activities. Formally dressed women in the corner watch the patients and whisper about them.
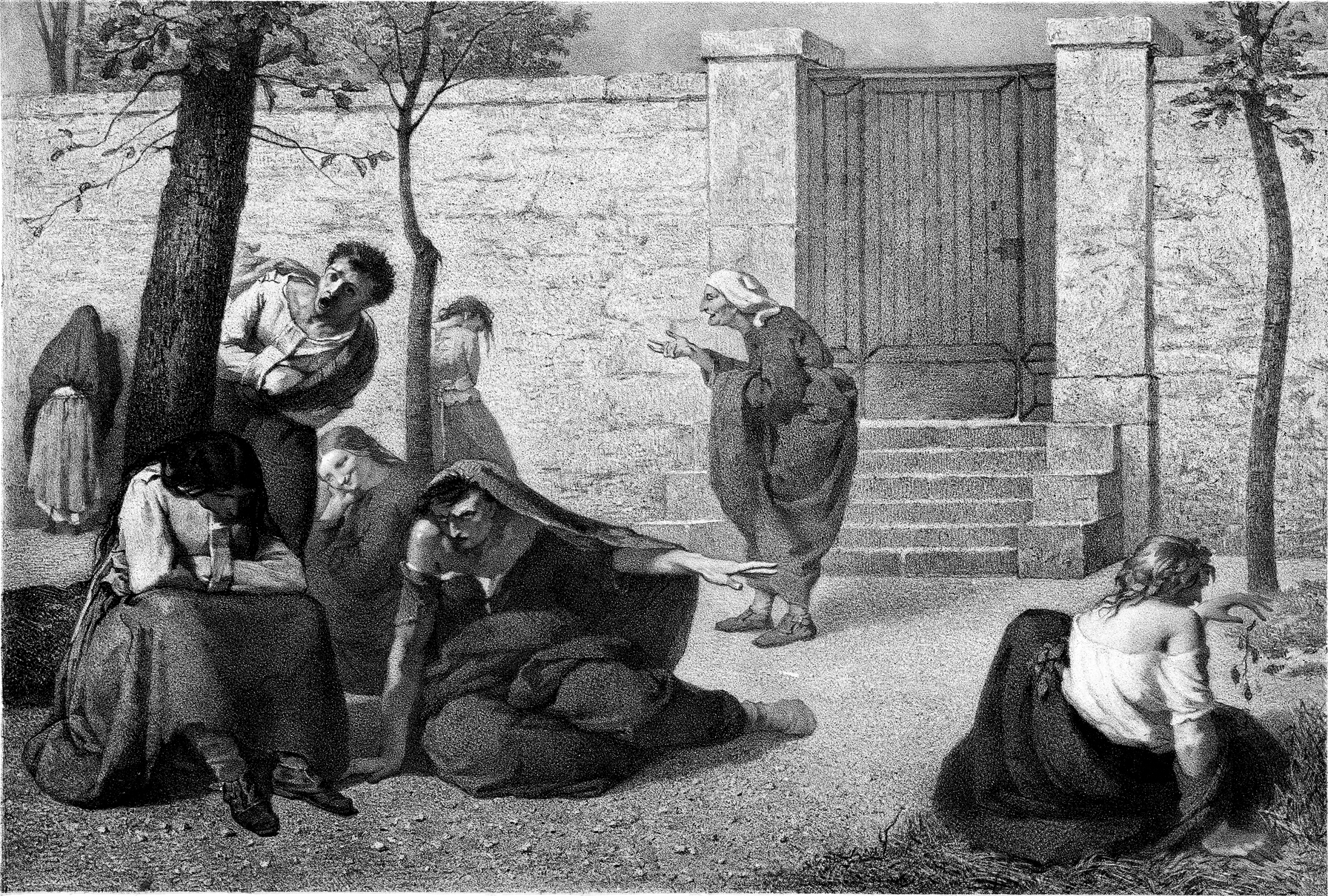
Figure 1.5 – Armand Gautier’s Madwomen of the Salpetriere is an 1857 lithograph intended to depict various conditions afflicting women found in the Salpetriere asylum. Each woman seems to be alone in her suffering and no caregivers are present.
To the extent that treatments were offered in early institutions, they were extremely primitive. At the time, the medical response to mental disorders was the same as that provided for physical illnesses. (Farreras) Bloodletting was one example of an early all-purpose treatment: a care provider would cut a nick in a vein or artery to allow removal of “excess” blood, supposedly increasing the health of the patient (Cohen, 2018).
Though the conditions in early institutions can be hard to fathom, they show us something about how this group of people were viewed. Authorities (including medical, legal, and moral leaders) believed that this group of people lacked the capacity to control themselves, and that along with that inability or lack of “reason,” it followed that they also lacked sensitivity to pain or misery. (Farreras) This is not so different from the startlingly recent belief that infants don’t feel pain – simply because they cannot verbalize or express it in a typically understood or “reasonable” way. This utterly false belief about infants was debunked in recent years with scientific evidence, but even through the 1980s this false belief encouraged surgeons to operate on young babies without providing any pain relief (University of Oxford, 2015).
1.2.3 Reforming Treatment of Mental Disorders
Fortunately, reformers in early 18th century Europe began thinking differently about how people with mental disorders were treated. Some doctors began to experiment with less restrictive practices for their patients. In Italy in the late 1700s, the physician Vincenzo Chiarughi began to unchain his patients at St. Boniface hospital in Florence – encouraging them to practice good hygiene and engage in recreational activity. Around the same time period, in France, physician Philippe Pinel famously unshackled his patients and actually talked to them at the Salpêtrière hospital in Paris (figure 1.6) (Micale, cited by Farreras).

Figure 1.6. This painting by Tony Robert-Fleury depicts Dr. Philippe Pinel ordering the removal of chains from patients at the Salpêtrière, a Paris asylum for women.
Pinel reportedly engaged in “therapeutic conversations” with patients, talking them through, or out of, their delusions. Though psychiatry was not yet an established medical field, and Pinel did not have many appealing options for medical treatment, he did recognize the need for treatment and offered what was available at the time: baths, opium, bloodletting, and occasional laxatives. Pinel, who would later be called the “father of modern psychiatry,” made lasting contributions to the treatment of those with mental disorders. He improved conditions in the Salpêtrière in particular, and modeled this for others. He also saw the occupants of those institutions as people in need of care, rather than simply dangerous threats to society who needed to be restrained (Tietz, 2021).
1.2.4 Licenses and Attributions for Historical Perspective on Mental Disorders
“Historical Perspective on Mental Disorders” by Anne Nichol is licensed under CC BY 4.0 but draws significantly from “Psychology 2e, 16.1- Mental Health Treatment: Past and Present ” by R. M. Spielman, W. J. Jenkins & M.D. Lovett, which is licensed under CC BY 4.0. Access for free at https://openstax.org/books/psychology-2e/pages/1-introduction. And Farreras – https://nobaproject.com/modules/history-of-mental-illness#content.
Figure 1.1. Photo of trephined skull, https://upload.wikimedia.org/wikipedia/commons/c/ce/Bronze_Age_skull_from_Jericho%2C_Palestine%2C_2200-2000_Wellcome_L0058402.jpg, See page for author, CC BY 4.0 <https://creativecommons.org/licenses/by/4.0>, via Wikimedia Commons.
Figure 1.2. Pius performing an exorcism. Exorcism | “Is not this the fast that I choose: to loose the… | Flickr.
Figure 1.3. “The Madhouse” by Francisco Goya is in the public domain. https://www.francisco-de-goya.com/madhouse/
Figure 1.4. William Hogarth’s Scene from Bedlam. https://www.flickr.com/photos/nlmhmd/51193077607/, in the public domain.
Figure 1.5. Armand Gautier’s Madwomen of the Salpetriere : Cushing/Whitney Medical Library : Library : Info : Image, Public Domain, https://commons.wikimedia.org/w/index.php?curid=12201396
Figure 1.6. “Pinel, médecin en chef de la Salpêtrière en 1795” by Tony Robert-Fleury is in the public domain.
