17 Chapter 17 – Sexual Dysfunction and Treatment
Ericka Goerling, PhD and Emerson Wolfe, MS
Learning Outcomes
- Apply the biopsychosocial approach in analyzing sexual dysfunctions.
- Distinguish various sexual dysfunctions under the umbrella of the DSM-V.
- Compare and contrast treatment options for sexual dysfunctions and ways to outreach to diverse community members.
Introduction
Movies and music videos often depict characters engaging in romantic, passionate sexual activity without challenges or inhibitions. Reality is often very different and conversations around sexual difficulties are sometimes met with shame, reducing their frequency and silencing individuals. However, sexual dysfunctions impact the lives of about 1 in 3 Americans (Fawcett & Crane, 2013). Instead of a one-size-fits-all model of sexual excitation and inhibition, further research has indicated that sexual arousal to internal (thoughts, fantasies, etc.) and external stimuli (images, touch, etc.) are based on individual traits, with some people being highly excitable while others experience reduced reactions (Rodriguez-Nieto et al., 2019). Arguably, sexual arousal operates similarly to other emotions in which a thought or experience produces arousal. Some individuals are more quick-tempered while others are more methodical and calm in their reactions. Biological, social, and psychological processes intersect to produce individuals’ responses, and a similar process can be seen in terms of sexual responsiveness. Additionally, for some people experiencing sexual dysfunctions, other underlying causes may be factors as well, such as anxiety, sexual trauma, depression, etc.
Terms have been developed, such as asexual, demisexual, sapiosexual, and more to explain how sexual attraction and sexual desire are complex processes. As with all human traits, sexual responsiveness exists on a continuum of possibilities rather than within a binary system in which sexual functioning equates health and a lack of sexual responsiveness equates disorder. At the same time, some people may want to be sexual and are distressed or experience relational difficulties when they face challenges. This unit will explore: the role of distress and impairment as a requirement for diagnosis, co-diagnosis and the importance of understanding underlying causes, the specific classifications of sexual dysfunctions (also known as disorders of sexual function) based on when they occur according to the sexual response cycle, the particular factors influencing sexual wellbeing for gender diverse individuals and sexual minorities, and sexual dysfunction treatments.
Distress and Impairment as a Diagnosis Requirement
In the DSM-5, sexual dysfunctions are defined as “a clinically significant disturbance in a person’s ability to respond sexually or to experience sexual pleasure” (American Psychiatric Association, 2013, p. 423). For some, sexual dysfunction has always been present whereas for others difficulties may develop later on in life. Additionally, individual differences may occur in which specific contexts cause dysfunction to arise or dysfunction can be present in all sexual situations for some people as well. More on this will be covered shortly. However, if significant distress is not present, then this is not considered a diagnosis. This is important because no one should be forced into being sexual if they do not want to be and sexual activity may be more distressing than not engaging in the behavior in some instances. Some people may have low sexual arousal or desire and are completely okay with this. Each person gets to decide their own unique sexual boundaries. If they do want to engage in sexual behavior but experience challenges, then this is when therapy can be useful. In the case of diagnosis, symptoms will need to be present for a minimum of six months, be present in 75% or more sexual situations in a persistent or recurrent fashion, and have caused the individual clinically significant distress (Mitchell et al., 2016).
Co-Diagnoses and Underlying Causes
Conducting a biopsychosocial assessment in which relationship factors, personal, cultural and religious beliefs, body image, underlying health concerns, mental health co-diagnoses, life stressors, and more can be explored to develop a comprehensive analysis of the many moving parts that may influence sexual wellbeing. For instance, conservative and stigmatized views regarding sexual behavior are associated with the development of sexual dysfunctions for individuals regardless of sexual orientation (Peixoto & Nobre, 2014). Mental health concerns, such as depression, anxiety, trauma, and more, can lead to the development of sexual difficulties (Basson & Gilks, 2018). Mitchell et al. (2016) found that individuals with one sexual dysfunction diagnosis, especially if experiencing a lack of interest or arousal disorder specifically, often met the criteria for additional sexual dysfunction diagnoses. Health concerns, such as high blood pressure, cancer, heart disease, etc., may also have the side effect of impacting sexual responsiveness, interest, and maintaining arousal. Medications for physical health as well as mental health concerns can have side effects that cause changes to sexual functioning, leading to the development of sexual dysfunctions. Exploring these underlying causes can aid the client and therapist (and medical doctor) in understanding the best treatment plan moving forward.
Disorders of Sexual Function
Sexual dysfunction is difficulty experienced by an individual or a couple during any stage of a normal sexual activity, including physical pleasure, desire, preference, arousal or orgasm. According to the DSM-5, sexual dysfunction requires a person to feel extreme distress and interpersonal strain for a minimum of six months (excluding substance or medication-induced sexual dysfunction). Sexual dysfunctions can have a profound impact on an individual’s perceived quality of sexual life. The term sexual disorder may not only refer to physical sexual dysfunction, but to paraphilias as well; this is sometimes termed disorder of sexual preference.
A thorough sexual history and assessment of general health and other sexual problems (if any) are very important. Assessing performance anxiety, guilt, stress and worry are integral to the optimal management of sexual dysfunction. Many of the sexual dysfunctions that are defined are based on the human sexual response cycle, proposed by William H. Masters and Virginia E. Johnson, and then modified by Helen Singer Kaplan, a psychologist and psychiatrist by training, who viewed human sexual response as a triphasic phenomenon, consisting of separate—but interlocking—phases: desire, arousal, and orgasm.
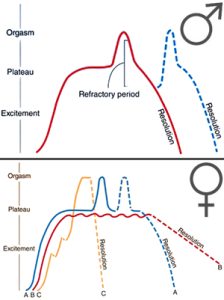
The Masters and Johnson research team pioneered research into the nature of human sexual response and the diagnosis and treatment of sexual disorders and dysfunctions from 1957 until the 1990s. One of the most enduring and important aspects of their work has been the four stage model of sexual response, which they described as the human sexual response cycle and defined as:
- Excitement phase (initial arousal)
- Plateau phase (at full arousal, but not yet at orgasm)
- Orgasm
- Resolution phase (after orgasm)
Their model shows no difference between Sigmund Freud’s purported categories of “vaginal orgasm” and “clitoral orgasm”: the physiological response was identical, even if the stimulation was in a different place.
Masters and Johnson’s findings also revealed that men undergo a refractory period following orgasm during which they are not able to ejaculate again, whereas there is no refractory period in women: this makes women capable of multiple orgasm. They also were the first to describe the phenomenon of the rhythmic contractions of orgasm in both sexes occurring initially in 0.8 second intervals and then gradually slowing in both speed and intensity.
The work of Masters and Johnson began in the Department of Obstetrics and Gynecology at Washington University in St. Louis and was continued at the independent not-for-profit research institution they founded in St. Louis in 1964, originally called the Reproductive Biology Research Foundation and renamed the Masters and Johnson Institute in 1978.
In the initial phase of Masters and Johnson’s studies, from 1957 until 1965, they recorded some of the first laboratory data on the anatomy and physiology of human sexual response based on direct observation of 382 women and 312 men in what they conservatively estimated to be “10,000 complete cycles of sexual response”. Their findings, particularly on the nature of female sexual arousal (for example, describing the mechanisms of vaginal lubrication and debunking the earlier widely held notion that vaginal lubrication originated from the cervix) and orgasm (showing that the physiology of orgasmic response was identical whether stimulation was clitoral or vaginal, and, separately, proving that some women were capable of being multiorgasmic), dispelled many long-standing misconceptions.
They jointly wrote two classic texts in the field, Human Sexual Response and Human Sexual Inadequacy, published in 1966 and 1970, respectively. Both of these books were best-sellers and were translated into more than thirty languages. The team has been inducted into the St. Louis Walk of Fame. Additionally, they are the focus of a television series called Masters of Sex for Showtime based on the 2009 biography by author Thomas Maier.
Their research into the anatomy and physiology of sexual response was a springboard to developing a clinical approach to the treatment of sexual problems in a revolutionary manner. Prior to 1970, when they described their treatment program to the world for the first time, sexual dysfunctions such as premature ejaculation, impotence, vaginismus, and female frigidity had been generally treated by long-term (multi-year) psychotherapy or psychoanalysis with very low rates of success. Masters and Johnson revolutionized things by devising a form of rapid treatment (2 week) psychotherapy always involving a couple, rather than just an individual, working with a male-female therapist team that resulted in a success rate of more than 80%. This was strictly a talking therapy – couples in their sex therapy program were never observed in sexual activity.
A more modern day approach to sexual response is the Dual Control Model of arousal, which is described by Emily Nagoski below:
Sexual disorders affect up to 43% of women and 31% of men (Laumann, Paik, & Rosen, 1999). Sexual disorders are often difficult to diagnose because in many cases the dysfunction occurs at the partner level (one or both of the partners are disappointed with the sexual experience) rather than at the individual level.
The sexual dysfunctions described in the DSM- 5 include delayed ejaculation, erectile disorder, female orgasmic disorder, female sexual interest/arousal disorder, genito-pelvic pain/penetration disorder, male hypoactive sexual desire disorder, premature (early) ejaculation, substance/medication-induced sexual dysfunction, other specified sexual dysfunction, and unspecified sexual dysfunction. See descriptions below.
| Disorder | Description |
| Male hypoactive sexual desire disorder(MHSDD) | Persistent or recurrently deficient sexual or erotic thoughts, fantasies, and desire for sexual activity. |
| Female sexual interest/arousal disorder | A complete lack of or significant reduction in sexual interest or sexual arousal. It is diagnosed with three or more of the following symptoms are manifested. These include the absence of an interest in sexual activity; or a decided reduction of such; and an absence of fantasizing or even thinking sexual or erotic thoughts. |
| Erectile disorder | Recurrent inability to achieve or maintain an adequate erection during partnered sexual activities. |
| Female orgasmic disorder | A significant change in orgasm such as delay, reduction of intensity or cessation. |
| Delayed ejaculation (DE) | Persistent difficulty or inability to achieve orgasm despite the presence of adequate desire, arousal, and stimulation. |
| Premature (early) ejaculation | Persistent or recurrent pattern of ejaculation occurring during partnered sexual activity within about one minute following vaginal penetration and before the individual wishes it. |
| Genito-pelvic pain/penetration disorder | Difficulty having intercourse and feeling significant pain upon penetration. |
| Substance/medication-induced sexual dysfunction | A condition in both men and women in which patients have difficulties with sexual desire, arousal, and/or orgasm due to a side effect of certain medications (legal or illicit). |
| Other specified sexual dysfunction, and unspecified sexual dysfunction | Used when symptoms of a sexual dysfunction are present and cause significant distress or impairment, but do not meet full criteria for any of the other disorders. |
Prevalence of Sexual Dysfunction in Men and Women. This chart shows the percentage of respondents who reported each type of sexual difficulty over the previous 12 months.
Sexual arousal disorders
Sexual arousal disorders were previously known as frigidity in women and impotence in men, though these have now been replaced with less judgmental terms. Impotence is now known as erectile dysfunction, and frigidity has been replaced with a number of terms describing specific problems that can be broken down into four categories as described by the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders: lack of desire, lack of arousal, pain during intercourse, and lack of orgasm.
For both men and women, these conditions can manifest themselves as an aversion to, and avoidance of, sexual contact with a partner. In men, there may be partial or complete failure to attain or maintain an erection, or a lack of sexual excitement and pleasure in sexual activity.
Hypoactive sexual desire disorder (HSDD) is considered a sexual dysfunction and is characterized as a lack or absence of sexual fantasies and desire for sexual activity, as judged by a clinician. For this to be regarded as a disorder, it must cause marked distress or interpersonal difficulties and not be better accounted for by another mental disorder, a drug (legal or illegal), or some other medical condition. A person with ISD will not start, or respond to their partner’s desire for, sexual activity. HSDD affects approximately 10% of all pre-menopausal women in the United States, or about 6 million women.
There are various subtypes. HSDD can be general (general lack of sexual desire) or situational (still has sexual desire, but lacks sexual desire for current partner), and it can be acquired (HSDD started after a period of normal sexual functioning) or lifelong (the person has always had no/low sexual desire.)
In the DSM-5, HSDD was split into male hypoactive sexual desire disorder (MHSDD) and female sexual interest/arousal disorder (FSIAD).
The DSM 5 has characterised the diagnostic features of male hypoactive sexual desire disorder (MHSDD) as males experiencing deficient or no erotic fantasies and desire for sexual activity for a period of at least 6 months. The level of deficiency in patients is determined by clinicians who take factors such as age and socio-cultural environment of the individual into account which may affect the individual’s sexual functioning. The manifestation of personal distress due to the disorder in the absence of non-sexual disorders, significant relationship stress, other forms of stress and other medical conditions distinguishes MHSDD. As with FSIAD, it can also be subdivided into the subtypes: lifelong, acquired, generalised, situational and distress severity can be classified as either: mild, moderate or severe.
Female sexual interest/arousal disorder is defined as the lack of or significantly reduced sexual interest/arousal with at least three of the following: absent/reduced interest in sexual activity; absent/reduced sexual/erotic thoughts or fantasies; no/reduced initiation of sexual activity, and typically unreceptive to a partner’s attempts to initiate; absent/reduced sexual excitement/pleasure during sexual activity in almost all or all (75 – 100%) sexual encounters (in identified situational contexts or, if generalized, in all contexts); absent/reduced sexual interest/arousal in response to any internal or external sexual/ erotic cues (e.g. written, verbal, visual); absent/reduced genital or non-genital sensations during sexual activity in almost all or all (75 – 100%) sexual encounters (in identified situational contexts or, if generalized, in all contexts).
Masters and Johnson were the first to conduct research on the sexual responsiveness of older adults, finding that given a state of reasonably good health and the availability of an interested and interesting partner, there was no absolute age at which sexual abilities disappeared. While they noted that there were specific changes to the patterns of male and female sexual responses with aging – for example, it takes older men longer to become aroused and they typically require more direct genital stimulation, and the speed and amount of vaginal lubrication tends to diminish with age as well – they noted that many older men and women are perfectly capable of excitement and orgasm well into their seventies and beyond, a finding that has been confirmed in population-based epidemiological research on sexual function in the elderly.
Men with erectile disorder cannot attain or maintain an erection during sexual activity that is sufficient to allow them to initiate or maintain sexual activity. The erectile dysfunction or impotence is a sexual dysfunction characterized by the inability to develop or maintain an erection of the penis. There are various underlying causes, such as damage to the nervi erigentes which prevents or delays erection, or diabetes as well as cardiovascular disease, which simply decreases blood flow to the tissue in the penis, many of which are medically reversible.
The causes of erectile dysfunction may be psychological or physical. Psychological erectile dysfunction can often be helped by almost anything that the patient believes in; there is a very strong placebo effect. Physical damage is much more severe. One leading physical cause of ED is continual or severe damage taken to the nervi erigentes. These nerves course beside the prostate arising from the sacral plexus and can be damaged in prostatic and colorectal surgeries.
Diseases are also common causes of erectile dysfunction; especially in men. Diseases such as cardiovascular disease, multiple sclerosis, kidney failure, vascular disease and spinal cord injury are the source of erectile dysfunction.
Due to its embarrassing nature and the shame felt by sufferers, the subject was taboo for a long time, and is the subject of many urban legends. Folk remedies have long been advocated, with some being advertised widely since the 1930s. The introduction of perhaps the first pharmacologically effective remedy for impotence, sildenafil (trade name Viagra), in the 1990s caused a wave of public attention, propelled in part by the news-worthiness of stories about it and heavy advertising.
It is estimated that around 30 million men in the United States and 152 million men worldwide suffer from erectile dysfunction. However, social stigma, low health literacy and social taboos lead to under reporting which makes an accurate prevalence rate hard to determine.
Orgasm disorders
Female orgasmic disorder refers to the inability to obtain orgasm in women. The woman enjoys sex and foreplay and shows normal signs of sexual arousal but cannot reach the peak experience of orgasm. Male orgasmic disorder refers to a delay in or absence of orgasm following a normal phase of excitement and an adequate degree of stimulation. Male orgasmic disorder is most often situational. The male may have an issue reaching orgasm with a certain partner, but not through masturbation. Male orgasmic disorder includes a delayed ejaculation (very rare) or (more commonly) premature ejaculation.
One of the most common sexual dysfunctions in men is premature ejaculation. It is not possible to exactly specify what defines premature, but if the man ejaculates before or immediately upon insertion of the penis into the vagina, most clinicians will identify the response as premature. Most men diagnosed with premature ejaculation ejaculate within one minute after insertion (Waldinger, 2003). Premature ejaculation is one of the most prevalent sexual disorders and causes much anxiety in many men.
Orgasm disorders, specifically anorgasmia, present as persistent delays or absence of orgasm following a normal sexual excitement phase in at least 75% of sexual encounters. The disorder can have physical, psychological, or pharmacological origins. SSRI antidepressants are a common pharmaceutical culprit, as they can delay orgasm or eliminate it entirely. A common physiological culprit of anorgasmia is menopause, where one in three women report problems obtaining an orgasm during sexual stimulation following menopause.
Sexual pain disorders
Genito-pelvic pain/penetration disorder (GPPPD) is a new diagnosis included in the 5th edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), which merged the revised definitions of both female sexual dysfunctions dyspareunia ( painful sex) and vaginismus (involuntary vaginal muscle spasms). At least one of the following persistent or recurrent criteria characterizes GPPPD: (1) difficulties with vaginal penetration during intercourse, (2) genito-pelvic pain during vaginal intercourse or penetration attempts, (3) fear or anxiety associated with genito-pelvic pain or vaginal penetration, or (4) tightness of the pelvic floor muscles during attempted vaginal penetration. One or more of these symptoms have to be present for at least 6 months and must cause clinically significant distress. GPPPD can be classified as either lifelong or acquired and, depending on the level of distress as mild, moderate or severe. The fusion of vaginismus and dyspareunia under a new classification and set of criteria was due to the significant overlap in clinical presentation, and exceeding difficulties to distinguish between the two reliably.
The prevalence of GPPPD has not been ascertained due to the novel criteria set. Reported prevalence rates in the general population vary between 3 and 25% for dyspareunia and 0.4 and 6.6% for vaginismus. Prevalence estimates are heterogeneous due to, e.g., varying diagnostic criteria, assessment methods, study design, and sample characteristics.
The burden of suffering associated with GPPPD and linked conditions such as vulvodynia and provoked vestibulodynia is high as symptoms have a detrimental impact on physiological and psychological health, and relational well-being. Vulvodynia is chronic pain in the vulva, the area on the outside of a woman’s genitals. It is usually described as a sensation of burning, stinging, itching or rawness. Vestibulodynia is chronic pain and discomfort that occurs in the area around the opening of the vagina, inside the inner lips of the vulva. This area is known as the vestibule.
GPPPD has been shown to have a negative effect on the women’s overall quality of life, with 60% of women reporting that the disorder compromised their ability to enjoy life. Moreover, it has been linked to depression and anxiety disorder. GPPPD symptoms are often comorbid with a wide range of other sexual dysfunctions and reduced sexual behavior. Many women with GPPPD also experience problems when using tampons or during gynecological examinations. GPPPD has been shown to contribute to declines in self-esteem and feelings of femininity and is associated with a negative body and genital self-image. It can pose a considerable burden on a couples’ relationship, especially if they would like to have children.
Sexual Dysfunctions and the LGBTQIA+ Community
As you can see from the previous section of the reading going over the classifications of the sexual dysfunctions, much of the research and language centers the experiences of cisgender and straight individuals. The particular contextual factors that influence the sexual functioning of gender diverse individuals and sexual minorities deserve specific attention.
Sexual Functioning and Gender Diversity
Nikkelen and Kreukels (2018) found that transgender individuals who desired gender-confirming care, such as hormones and/or surgery, and received these services experienced increases in sexual satisfaction and sexual wellbeing. Individuals who desired services but were unable to receive them reported less body satisfaction and less sexual satisfaction. People who did not desire transition services were the most satisfied with their bodies and with their sexual behaviors. Thus, the role of body satisfaction can be seen as having an impact on sexual functioning and satisfaction. Body satisfaction was somewhat more important to the transgender women participants in relation to their sexual wellbeing than the transgender men participants as a whole. This research is important to understand that some transgender individuals may desire hormones and/or surgeries more than others and that body satisfaction plays an important role in sexual functioning (Nikkelen & Kreukels, 2018). Unfortunately, research is lacking regarding the experiences of gender-expansive, gender non-conforming, and gender non-binary individuals.
Sexual Functioning and Sexual Minorities
Li et al. (2019) found that internalized stigma and shame related to sexual orientation was associated with less sexual satisfaction in the study of participants who identified as men who have sex with men (both gay and bisexual men were included together). If the participants perceived the neighborhood in which they lived to be accepting of their sexual orientation, then this was correlated with higher levels of sexual satisfaction as well. This indicates that internalized and social stigma may have an impact on some individuals’ sexual wellbeing. Shindel et al. (2012) found no significant statistical difference between the incidence of sexual dysfunctions between men who have sex with men and straight men. The same factors that increased the chance of sexual dysfunctions in straight men, such as increasing age, underlying health concerns, urinary tract issues and lack of a consistent, stable romantic relationship, impacted men who have sex with men as well (Shindel et al., 2012).
Stereotypes exist regarding lesbian sexual behaviors and desire in which the term “lesbian bed death” derives, meaning that after a few years of being in a relationship, lesbians will no longer engage in sexual behaviors with each other (Peixoto & Nobre, 2014, p. 2691). However, the reality lies in how women are socialized to be more passive regarding sex causing them to initiate less frequently. Understanding the influence of gender socialization and sexual scripts in the lives of lesbian women can be helpful instead. For instance, Peixoto and Nobre (2014) found that the biggest factor in influencing the development of sexual dysfunctions in both straight and lesbian women was internalizing the belief that sexual desire and pleasure are sins.
Theories and Treatment of Sexual Dysfunctions
Sexual dysfunctions have a variety of causes. In some cases the primary problem is biological, and the disorder may be treated with medication. Other causes include a repressive upbringing in which the parents have taught the person that sex is dirty or sinful, or the experience of sexual abuse (Beitchman, Zucker, Hood, & DaCosta, 1992). In some cases the sex problem may be due to the fact that the person has a different sexual orientation than he or she is engaging in. Other problems include poor communication between the partners, a lack of sexual skills, and (particularly for men) performance anxiety.
It is important to remember that most sexual disorders are temporary — they are experienced for a period of time, in certain situations or with certain partners, and then (without, or if necessary with, the help of therapy) go away. It is also important to remember that there are a wide variety of sex acts that are enjoyable. Couples with happy sex lives work together to find ways that work best for their own styles. Sexual problems often develop when the partners do not communicate well with each other, and are reduced when they do.
Sexual arousal disorders

Contrary to popular belief, sexual arousal disorder is not always caused from a lack of sexual arousal. Possible causes of the disorder include psychological and emotional factors, such as depression, anger, and stress; relationship factors, such as conflict or lack of trust; medical factors, such as depleted hormones, reduced regional blood flow, and nerve damage; and drug use. The lack of sexual arousal may be due to a general lack of sexual desire or due to a lack of sexual desire for the current partner (i.e., situational). A person may always have had no or low sexual desire or the lack of desire may have been acquired during the person’s life. Certain medications like SSRIs may be a contributing factor.
Treatment depends on the cause of the disorder. Hormone therapy or a blood-flow enhancing medication, like Viagra, may be appropriate. Bremelanotide (formerly PT-141) is being studied in clinical tests to increase sexual desire in women. In 2014, Palatin, the company developing the drug, announced the beginning of a Phase 3 clinical trial to determine its effectiveness. Flibanserin, sold under the trade name Addyi, is a medication approved for the treatment of pre-menopausal women with hypoactive sexual desire disorder (HSDD).
Disorders Involving Orgasm
The condition is sometimes classified as a psychiatric disorder. However, it can also be caused by medical problems such as diabetic neuropathy, multiple sclerosis, genital mutilation on either gender, complications from genital surgery, pelvic trauma (such as from a straddle injury caused by falling on the bars of a climbing frame, bicycle or gymnastics beam), hormonal imbalances, total hysterectomy, spinal cord injury, cauda equina syndrome, uterine embolisation, childbirth trauma (vaginal tearing through the use of forceps or suction or a large or unclosed episiotomy), vulvodynia and cardiovascular disease.
Primary anorgasmia is a condition where one has never experienced an orgasm. This is significantly more common in women, although it can occur in men who lack the gladipudendal (bulbocavernosus) reflex. Women with this condition can sometimes achieve a relatively low level of sexual excitement. Frustration, restlessness, and pelvic pain or a heavy pelvic sensation may occur because of vascular engorgement. On occasion, there may be no obvious reason why orgasm is unobtainable. In such cases, women report that they are unable to orgasm even if they have a caring, skilled partner, adequate time and privacy, and an absence of medical issues which would affect sexual satisfaction.
About 15% of women report difficulties with orgasm, and as many as 10% of women in the United States have never climaxed. Only 29% of women always have orgasms with their partner.
Secondary anorgasmia is the loss of the ability to have orgasms (as opposed to primary anorgasmia which indicates a person who has never had an orgasm). Or loss of the ability to reach orgasm of past intensity. The cause may be alcoholism, depression, grief, pelvic surgery (such as total hysterectomy) or injuries, certain medications, death-grip, illness, estrogen deprivation associated with menopause, or rape.
Orgasmic dysfunction is more prevalent in younger and less sexually experienced women. Primary (life-long) anorgasmia is found in about 5-10% of women and is less common than secondary (acquired) anorgasmia.
Research has shown that almost two-thirds of women have concerns about their sexual relationships. In a study in America 43% of the 1749 women interviewed reported experiencing in the past year events such as a lack of interest in sex, inability to achieve orgasm and trouble lubricating compared with 31% of men.
Many factors affect orgasmic function, e.g. age, education, job, folklore (taboos), religious beliefs, drugs, psychological disorders and gynecological surgery.
Sexual dysfunction causes many problems for couples; some researchers found that up to 67% of divorces are related to sexual disorders. It seems that counseling and education in sexual behavior is the most effective treatment for sexual dysfunction.
Genito-Pelvic Pain/Penetration Disorder
Regarding the broad symptom profile of GPPPD, its etiology and maintenance can be best explained by a biopsychosocial framework considering a wide range of interdependent pathophysiological, psychological, social, cultural, and relational factors as well as critical life events. According to the fear-avoidance model, maladaptive cognitions including worrying about losing control of one’s body, genital incompatibility, and pain catastrophizing are crucial in maintaining and reinforcing genito-pelvic pain and associated GPPPD symptoms, by leading to fear and hypervigilance in sexual situations, or complete avoidance of sexual intimacy. Beyond individual aspects, relationship dynamics such as dyadic communication and stress coping, as well as partners’ responses have been shown to have profound influence on GPPPD symptoms. To an appreciable extent, GPPPD has also been found to concur with male partners’ sexual dysfunctions.
Due to the biopsychosocial nature of GPPPD, a multidimensional integrative treatment approach is needed that targets not only difficulties with vaginal penetration, pain, anxiety, and muscle tightness associated with sexual intercourse but also sexual satisfaction and couple dynamics. Psychological interventions for vaginismus and dyspareunia include strategies such as pain management, systematic desensitization, cognitive restructuring, pelvic-floor exercises, sensate focus, and mindfulness. Only few interventions, however, have been empirically tested so far. Of these trials, only few studies have applied randomized controlled trial (RCT) design, most of them with only small sample sizes. Findings of these RCTs indicate that psychological treatments can result in significant improvement of intercourse penetration ability, decrease in pain during intercourse, and higher levels of sexual functioning. However, none of these studies targeted all symptoms of GPPPD.
Sex Therapy
Sex therapy is a strategy for the improvement of sexual function and treatment of sexual dysfunction. This includes sexual dysfunctions such as premature ejaculation or delayed ejaculation, erectile dysfunction, lack of sexual interest or arousal, and painful sex. It includes dealing with problems imposed by atypical sexual interests (paraphilias), gender dysphoria and being transgender; highly overactive libido or hypersexuality, a lack of sexual confidence, recovering from sexual abuse, such as rape, sexual assault, and sexual issues related to aging, illness, or disability.
It can include sensate focus, communication, and fantasy exercises as well as psychodynamic therapy. Sensate focus is a sex therapy technique introduced by the Masters and Johnson team. It works by refocusing the participants on their own sensory perceptions and sensuality, instead of goal-oriented behavior focused on the genitals and penetrative sex. Sensate focus has been used to treat problems with body image, erectile dysfunction, orgasm disorders, and lack of sexual arousal.
The exercises are conducted by the couple at home, between therapy sessions. Although the couple are nude and touching each other during the exercises, they are instructed to abstain from sexual intercourse during or close to the sessions. Both participants are instructed instead to focus on their own varied sense experience, instead of focusing on performance or orgasm. Initially, the emphasis is on touching in a mindful way for oneself without regard for sexual response or pleasure for oneself or one’s partner.
The second stage increases the touch options to include breasts. Sensation and gathering information about the partner’s body is still encouraged and intercourse and touching of the genitals is still forbidden. The participants then use a technique of placing their hand over their partner’s hand in order to show what they find pleasurable in terms of pace and pressure. Learning about the partner’s body is still the goal rather than pleasure. Further stages gradually re-introduce touching of breasts and genitals, then intercourse. Orgasm is never the focus.
Cognitive Sexual Therapy
Cognitive-behavioral therapy is recognized by its efforts in developing and providing evidence-based psychotherapeutic interventions to various kinds of psychological and interpersonal problems, being this ideological standpoint a trigger to continuous actualization of its theory and practice. Cognitive sexual therapy (CST) is a cognitive-behavioral integrative psychotherapy aimed specifically to address and treat SDs, articulating evidence-based clinical interventions to scientific understandings of human sexuality. In a CST perspective, distorted sexual cognitions, allied to individuals´ misinterpretations of sexual demands, directly affect emotional, physiological and behavioral regulation in sexual situations. In this sense, restructuring central and intermediate cognitive processes is essential to foster the acquisition of sexual skills and to promote the development of a more adapted sexual repertoire. Thus, cognitions are understood as mediating factors to be modified, aiming sexual skills implementation and emotional regulation during sexual encounters.
Sexual Scripts are ideas of how males and females are supposed to interact with each other, including how each gender should behave in sexual or romantic situations. Being able to flex sexual scripts and behaviors leads to better adaptation to physiological, environmental and relational changes that negatively impact sexuality over the life cycle, contributing to booster sexual satisfaction even in the presence of sexual function disturbances. The focus of CST interventions is to aid patients and partners towards the development of more flexible and adaptable sexual cognitions and behavioral patterns. CST could permit a regain in sexual function and satisfaction during and after treatment with psychotropic medication, lessen the negative impact of sexual adverse effects in quality of life and therefore, increase adherence and therapeutic effects of pharmacotherapy. Although the theoretical rationale supporting this proposal is evidence-based, feasibility, efficacy, treatment modalities and procedural aspects of the intervention remain to be empirically tested.
Conclusion
Sexual dysfunctions are complex issues that affect a significant portion of the population, impacting individuals across various demographics and sexual orientations. We’ve examined how these issues are defined, diagnosed, and treated, emphasizing the importance of a biopsychosocial approach that considers the whole person and their unique circumstances. Treatment options for sexual dysfunctions have evolved significantly, ranging from pharmacological interventions to various forms of therapy, but more work can be done. The importance of communication, both between partners and with healthcare providers, cannot be overstated in addressing these issues effectively.
As our understanding of human sexuality continues to grow, so too does our ability to address sexual dysfunctions in a compassionate, effective, and inclusive manner. Moving forward, it’s crucial to continue research in this field, challenge societal norms that may contribute to sexual difficulties, and promote open dialogue about sexual health. By doing so, we can work towards a future where individuals of all backgrounds can achieve sexual well-being and satisfaction.
Reflection Questions
- This chapter discusses how sexual dysfunctions are defined in terms of causing “clinically significant distress.” How might societal expectations and cultural norms influence what is considered “normal” sexual functioning versus a dysfunction? Can you think of any potential issues with this approach to diagnosis?
- The reading mentions that many sexual dysfunctions can be temporary or situation-specific. How might this information impact the way we view and treat sexual problems? What are some potential benefits and drawbacks of this perspective?
- Consider the section on sexual dysfunctions in the LGBTQIA+ community. How might the experiences and challenges faced by gender diverse individuals and sexual minorities differ from those of cisgender and heterosexual individuals when it comes to sexual functioning? What are some ways healthcare providers could better address these specific needs?
- We outline various treatment approaches for sexual dysfunctions, including medication, therapy, and lifestyle changes. How might a biopsychosocial approach be beneficial in addressing sexual dysfunctions? Can you think of any potential limitations to this approach?
- Reflect on the role of communication in sexual functioning, as mentioned in the chapter. How might improving communication between partners potentially prevent or alleviate some sexual dysfunctions? What barriers might exist to open communication about sexual issues?
Additional Resources
- From OHSU: “Sexual Medicine 101/201: Treating Low Libido in Women” (Adams, 2019)
- From Standford Medicine: “Disaggregating gender from sex in sexual dysfunction epidemiology.” (Obedin-Maliver, 2020)
Licenses & Attributions
Clinical Perspectives in Abnormal Psychology by Sonja Ann Miller is licensed under Creative Commons BY 4.0 Lumen Learning (2020). Abnormal psychology. Retrieved from https://courses.lumenlearning.com/hvcc-abnormalpsychology/
Adaptations: Reformatted. Added learning objectives. Modified content for language, application to subject and cohesion. Updated sources.
All Rights Reserved
Dr. Tracy Marks (2019, January 2). Why antidepressants kill your sex drive – and what to do about it [Video]. https://www.youtube.com/watch?v=Kj1WQM37YR8. License: All Rights Reserved. License Terms: Standard YouTube license.
Howcast (2012, July 12). What happens in a sex therapy session? Psychology of sex [Video]. https://www.youtube.com/watch?v=JYwLvpAAW20. License: All Rights Reserved. License Terms: Standard YouTube license.
Nagoski, E. (2016, February 12). Confidence and joy are the keys to a great sex life [Video]. TEDx University of Nevada. https://www.youtube.com/watch?v=HILY0wWBlBM License: All Rights Reserved. License Terms: Standard YouTube license.
Ohio State Wexner Medical Center (2016, October 24). The importance of early treatment for erectile dysfunction [Video]. https://www.youtube.com/watch?v=AHTRNoHqQNM. License: All Rights Reserved. License Terms: Standard YouTube license.
Pelvic Health and Rehabilitation Center (2020, December 29). Vulvodynia, vestibulodynia, vaginismus… What’s the difference [Video]? https://www.youtube.com/watch?v=jhn_gzrv_ns. License: All Rights Reserved. License Terms: Standard YouTube license.
References
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). https://doi.org/10.1176/appi.books.9780890425596
Basson, R., & Gilks, T. (2018). Women’s sexual dysfunction associated with psychiatric disorders and their treatment. Women’s Health. https://doi.org/10.1177/1745506518762664
Li, D. H., Remble, T. A., Macapagal, K., & Mustanski, B. (2019). Stigma on the streets, dissatisfaction in the sheets: Is minority stress associated with decreased sexual functioning among young men who have sex with men?. The Journal of Sexual Medicine, 16(2), 267–277. https://doi.org/10.1016/j.jsxm.2018.12.010
Miller, S. A. (2020). Clinical perspectives in abnormal psychology. Lumen Learning. Retrieved from https://courses.lumenlearning.com/hvcc-abnormalpsychology/
Mitchell, K. R., Jones, K. G., Wellings, K., Johnson, A. M., Graham, C. A., Datta, J., Copas, A. J., Bancroft, J., Sonnenberg, P., Macdowall, W., Field, N., & Mercer, C. H. (2016). Estimating the prevalence of sexual function problems: The impact of morbidity criteria. Journal of Sex Research, 53(8), 955–967. https://doi.org/10.1080/00224499.2015.1089214
Nikkelen, S. W. C., & Kreukels, B. P. C. (2018). Sexual experiences in transgender people: The role of desire for gender-confirming interventions, psychological well-being, and body satisfaction. Journal of Sex & Marital Therapy, 44(4), 370–381. https://doi-org.libproxy.pcc.edu/10.1080/0092623X.2017.1405303
Peixoto, M. M., & Nobre, P. (2014). Dysfunctional sexual beliefs: A comparative study of heterosexual men and women, gay men, and lesbian women with and without sexual problems. The Journal of Sexual Medicine, 11(11), 2690–2700. https://doi.org/10.1111/jsm.12666
Rodriguez-Nieto, G., Emmerling, F., Dewitte, M., Sack, A. T., & Schuhmann, T. (2019). The role of inhibitory control mechanisms in the regulation of sexual behavior. Archives of Sexual Behavior, 48(2), 481–494. https://doi.org/10.1007/s10508-018-1283-7
Shindel, A. W., Vittinghoff, E., & Breyer, B. N. (2012). Erectile dysfunction and premature ejaculation in men who have sex with men. The Journal of Sexual Medicine, 9(2), 576–584. https://doi.org/10.1111/j.1743-6109.2011.02585.x

