6.3 Environmental Health
Section Goals:
- Define environmental health.
- Discuss the interconnection between poverty and health, which is a major impact on child health and survival.
- Discuss emerging diseases as a part of environmental health.
- Highlight the importance and risk of antibiotic resistance.
Environmental Health
Environmental health is concerned with preventing disease, death and disability by reducing exposure to adverse environmental conditions and promoting behavioral change. It focuses on the direct and indirect causes of diseases and injuries, and taps resources inside and outside the health care system to help improve health outcomes.
Poverty, Health and Environment
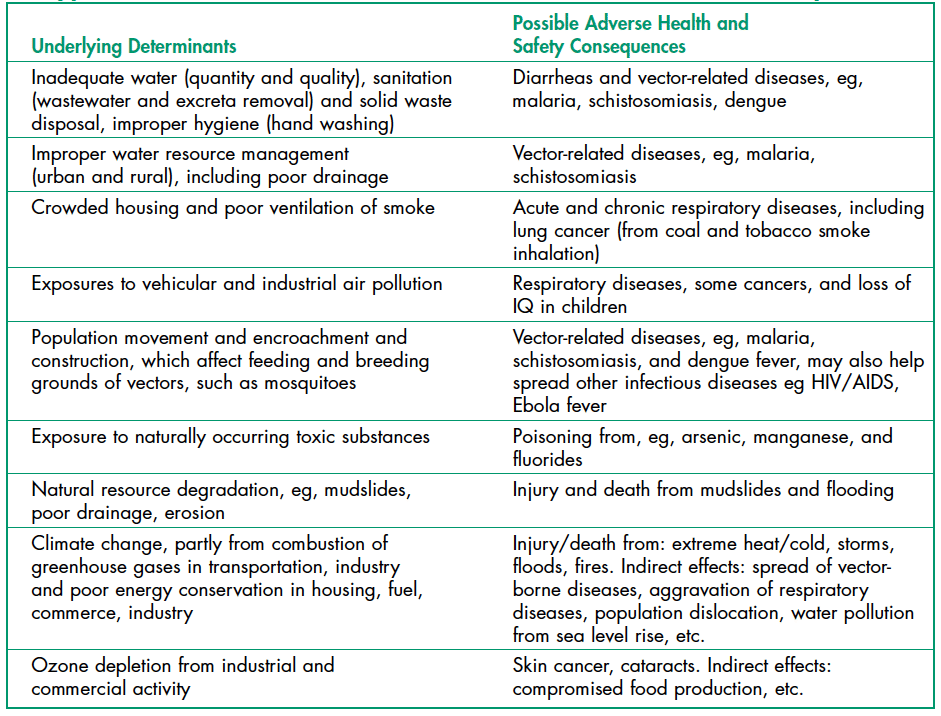
Environmental health risks can be grouped into two broad categories. Traditional hazards are related to poverty and the lack of development and mostly affect developing countries and poor people. Their impact exceeds that of modern health hazards by 10 times in Africa, 5 times in Asian countries (except for China), and 2.5 times in Latin America and Middle East (Figure 1). Water-related diseases caused by inadequate water supply and sanitation impose an especially large health burden in Africa, Asia, and the Pacific region. In India alone, over 700,000 children under 5 die annually from diarrhea. In Africa, malaria causes about 500,000 deaths annually. More than half of the world’s households use unprocessed solid fuels, particularly biomass (crop residues, wood, and dung) for cooking and heating in inefficient stoves without proper ventilation, exposing people—mainly poor women and children—to high levels of indoor air pollution(IAP). IAP causes about 2 million deaths in each year.
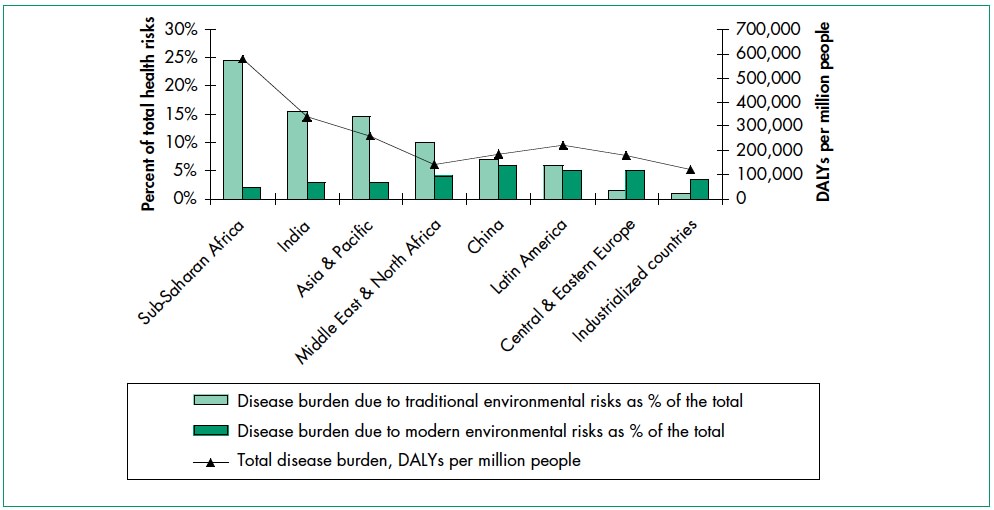
Modern hazards, caused by technological development, prevail in industrialized countries where exposure to traditional hazards is low. The contribution of modern environmental risks to the disease burden in most developing countries is similar to – and in quite a few countries, greater than – that in rich countries. Urban air pollution, for example, is highest in parts of China, India and some cities in Asia and Latin America. Poor people increasingly experience a “double burden” of traditional and modern environmental health risks. Their total burden of illness and death from all causes per million people is about twice that in rich countries, and the disease burden from environmental risks is 10 times greater.
Environmental Health and Child Survival
Worldwide, the top killers of children under five are acute respiratory infections (from indoor air pollution); diarrheal diseases (mostly from poor water, sanitation, and hygiene); and infectious diseases such as malaria. Children are especially susceptible to environmental factors that put them at risk of developing illness early in life. Four specific examples are highlighted here: Malnutrition, Poor Sanitation, Indoor Air Pollution, and Malaria.
Malnutrition
Malnutrition (the condition that occurs when body does not get enough nutrients) is an important contributor to child mortality—malnutrition and environmental infections are inextricably linked. The World Health Organization (WHO) recently concluded that about 50% of the consequences of malnutrition are in fact caused by inadequate water and sanitation provision and poor hygienic practices.
Poor Water and Sanitation Access
With 1.1 billion people lacking access to safe drinking water and 2.6 billion without adequate sanitation, the magnitude of the water and sanitation problem remains significant. Each year contaminated water and poor sanitation contribute to 5.4 billion cases of diarrhea worldwide and 1.6 million deaths, mostly among children under the age of five. Intestinal worms, which thrive in poor sanitary conditions, infect close to 90 percent of children in the developing world and, depending on the severity of the infection may lead to malnutrition, anemia, or stunted growth. About 6 million people are blind from trachoma, a disease caused by the lack of clean water combined with poor hygiene practices.
Indoor Air Pollution
Indoor air pollution—a much less publicized source of poor health—is responsible for more than 1.6 million deaths per year and for 2.7% of global burden of disease. It is estimated that half of the world’s population, mainly in developing countries, uses solid fuels (biomass and coal) for household cooking and space heating. Cooking and heating with such solid fuels on open fires or stoves without chimneys lead to indoor air pollution and subsequently, respiratory infections. Exposure to these health-damaging pollutants is particularly high among women and children in developing countries, who spend the most time inside the household. As many as half of the deaths attributable to indoor use of solid fuel are of children under the age of five.
Malaria
Approximately 40% of the world’s people—mostly those living in the world’s poorest countries—are at risk from malaria. Malaria is an infectious disease spread by mosquitoes but caused by a single-celled parasite called Plasmodium. Every year, more than 200 million people become infected with malaria and about 430,000 die, with most cases and deaths found in Sub-Saharan Africa. However, Asia, Latin America, the Middle East, and parts of Europe are also affected. Pregnant women are especially at high risk of malaria. Non-immune pregnant women risk both acute and severe clinical disease, resulting in fetal loss in up to 60% of such women and maternal deaths in more than 10%, including a 50% mortality rate for those with severe disease. Semi-immune pregnant women with malaria infection risk severe anemia and impaired fetal growth, even if they show no signs of acute clinical disease. An estimated 10,000 women and 200,000 infants die annually as a result of malaria infection during pregnancy.
Emerging Diseases
Emerging and re-emerging diseases have been defined as infectious diseases of humans whose occurrence during the past two decades has substantially increased or threatens to increase in the near future relative to populations affected, geographic distribution, or magnitude of impacts. Examples include Ebola virus, West Nile virus, Zika virus, sudden acute respiratory syndrome (SARS), H1N1 influenza; swine and avian influenza (swine, bird flu), HIV, and a variety of other viral, bacterial, and protozoal diseases.
A variety of environmental factors may contribute to re-emergence of a particular disease, including temperature, moisture, human food or animal feed sources, etc. Disease re-emergence may be caused by the coincidence of several of these environmental and/or social factors to allow optimal conditions for transmission of the disease.
Ebola, previously known as Ebola hemorrhagic fever, is a rare and deadly disease caused by infection with one of the Ebola virus strains. Ebola can cause disease in humans and nonhuman primates. The 2014 Ebola epidemic is the largest in history (with over 28,000 cases and 11,302 deaths), affecting multiple countries in West Africa. There were a small number of cases reported in Nigeria and Mali and a single case reported in Senegal; however, these cases were contained, with no further spread in these countries.
The HIV/AIDS epidemic has spread with ferocious speed. Virtually unknown 20 years ago, HIV has infected more than 60 million people worldwide. Each day, approximately 14,000 new infections occur, more than half of them among young people below age 25. Over 95 percent of PLWHA (People Living With HIV/AIDS) are in low- and middle- income countries. More than 20 million have died from AIDS, over 3 million in 2002 alone. AIDS is now the leading cause of death in Sub-Saharan Africa and the fourth-biggest killer globally. The epidemic has cut life expectancy by more than 10 years in several nations.
It seems likely that a wide variety of infectious diseases have affected human populations for thousands of years emerging when the environmental, host, and agent conditions were favorable. Expanding human populations have increased the potential for transmission of infectious disease as a result of close human proximity and increased likelihood for humans to be in “the wrong place at the right time” for disease to occur (e.g., natural disasters or political conflicts). Global travel increases the potential for a carrier of disease to transmit infection thousands of miles away in just a few hours, as evidenced by WHO precautions concerning international travel and health.
Antibiotic Resistance
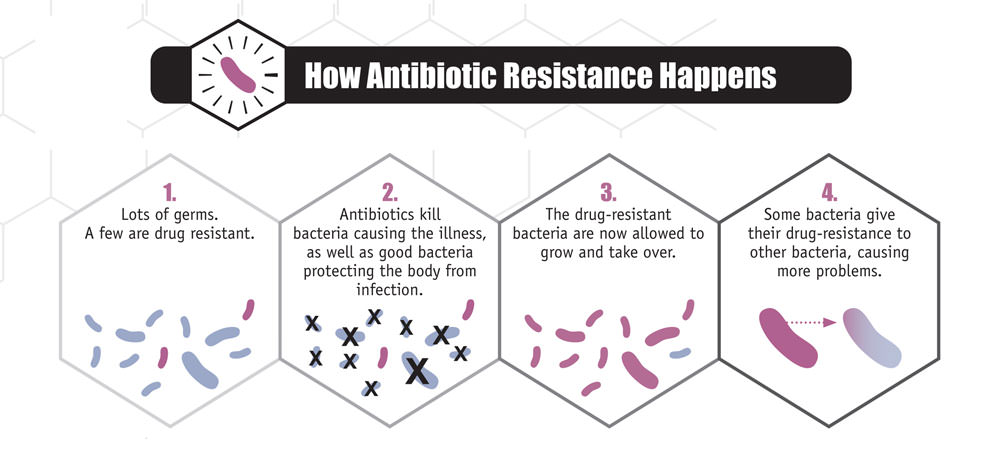
Antibiotics and similar drugs, together called antimicrobial agents, have been used for the last 70 years to treat patients who have infectious diseases. Since the 1940s, these drugs have greatly reduced illness and death from infectious diseases. However, these drugs have been used so widely and for so long that the infectious organisms the antibiotics are designed to kill have adapted to them, making the drugs less effective. Antibiotic resistance occurs when bacteria change in a way that reduces the effectiveness of drugs, chemicals, or other agents designed to cure or prevent infections. This is caused by the process of evolution through natural selection (Figure 3). The antibiotic-resistant bacteria survive and continue to multiply, causing more harm.
New forms of antibiotic resistance can cross international boundaries and spread between continents with ease. Many forms of resistance spread with remarkable speed. Each year in the United States, at least 2 million people acquire serious infections with bacteria that are resistant to one or more of the antibiotics designed to treat those infections. At least 23,000 people die each year in the US as a direct result of these antibiotic-resistant infections. Many more die from other conditions that were complicated by an antibiotic-resistant infection. The use of antibiotics is the single most important factor leading to antibiotic resistance around the world.

Antibiotics are among the most commonly prescribed drugs used in human medicine, but up to 50% of all the antibiotics prescribed for people are not needed or are not optimally effective as prescribed.
During recent years, there has been growing concern over methicillin-resistant Staphylococcus aureus (MRSA), a bacterium that is resistant to many antibiotics. In the community, most MRSA infections are skin infections. In medical facilities, MRSA causes life-threatening bloodstream infections, pneumonia and surgical site infections.
Suggested Supplementary Reading:
Koch, B.J. et al. 2017. Food-animal production and the spread of antibiotic resistance: the role of ecology. Frontiers in Ecology and the Environment (15)6: 309-318.
Notable Excerpts:
“Antibiotic use in food animals is correlated with antibiotic resistance among bacteria affecting human populations.” p. 311
“Microbial genes encoding antibiotic resistance have moved between the food-animal and human health sectors, resulting in illnesses that could not be treated by antibiotics.” p. 312
Attribution
Essentials of Environmental Science by Kamala Doršner is licensed under CC BY 4.0. Modified from the original by Matthew R. Fisher and Joni Baumgarten.

