Vitamins and Minerals Involved in Blood Health
Blood is essential to life. It transports absorbed nutrients and oxygen to cells, removes metabolic waste products for excretion, and carries molecules, such as hormones, to allow for communication between organs.
Blood is a connective tissue of the circulatory system, made up of four components forming a matrix:
- red blood cells (or erythrocytes), which transport oxygen to cells
- white blood cells (or leukocytes), which are part of the immune system and help destroy foreign invaders
- platelets, which are fragments of cells that circulate to assist in blood clotting
- plasma, which is the fluid portion of the blood and contains proteins that help transport nutrients (e.g., fat-soluble vitamins) and aid in blood clotting.
Maintaining healthy blood, including its continuous renewal, is essential to support its vital functions. Blood health is acutely sensitive to deficiencies in some vitamins and minerals, especially iron and vitamin K.
Iron
Iron is a trace mineral. It is a necessary component of many proteins in the body responsible for functions such as the transport of oxygen, energy metabolism, immune function, and antioxidant defense. Iron is also important in brain development and function.
Iron is essential for oxygen transport because of its role in hemoglobin, a protein in red blood cells that transports oxygen to cells and gives red blood cells their color. Hemoglobin is composed of four globular peptides, each with an iron-containing heme complex in the center (Figure 9.19).
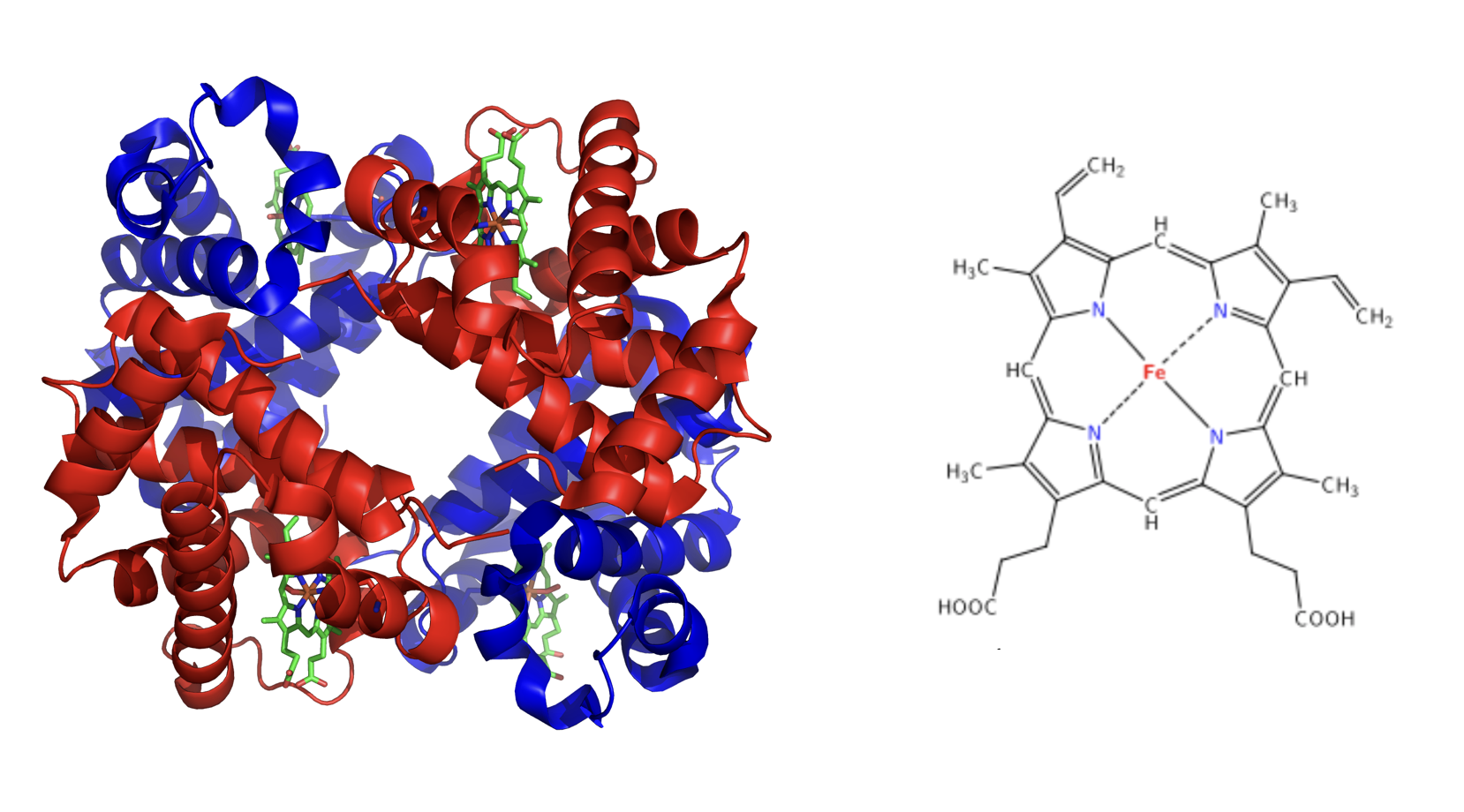
Figure 9.19. The structure of hemoglobin and the heme complex. On the left, the structure of hemoglobin includes four globular peptides (shown in blue and red) and the iron-containing heme groups (shown in green). On the right is a closer view of the heme complex.
The iron in hemoglobin is what binds to oxygen, allowing for transportation to cells. If iron levels are low, hemoglobin is not synthesized in sufficient amounts, and the oxygen-carrying capacity of red blood cells is reduced, resulting in anemia. Iron is also an important part of myoglobin, a protein similar to hemoglobin but found in muscles.
Dietary Sources of Iron
There are two types of iron found in foods: heme iron and non-heme iron.
- Heme iron is iron that is part of the proteins hemoglobin and myoglobin, so it is found only in foods of animal origin, such as meat, poultry, and fish. Heme iron is the most bioavailable form of iron. About 40% of the iron in animal foods is heme iron and 60% is non-heme iron.
- Non-heme iron is the mineral by itself and is not a part of hemoglobin or myoglobin. Non-heme iron can be found in foods from both plants (e.g., nuts, beans, vegetables, and fortified and whole grains) and animals. It is less bioavailable than heme iron. Consuming vitamin C, meat, poultry, and seafood with non-heme iron increases its bioavailability. For example, eating an orange ( a good source of vitamin C) along with your bowl of vegetarian chili will help you to absorb more of the iron from the beans and vegetables. On the other hand, chemicals such as phytates (found in beans and grains) and plant polyphenols (found in fruits, vegetables, some cereals, legumes, tea, coffee, and wine) decrease bioavailability due to binding with iron.1
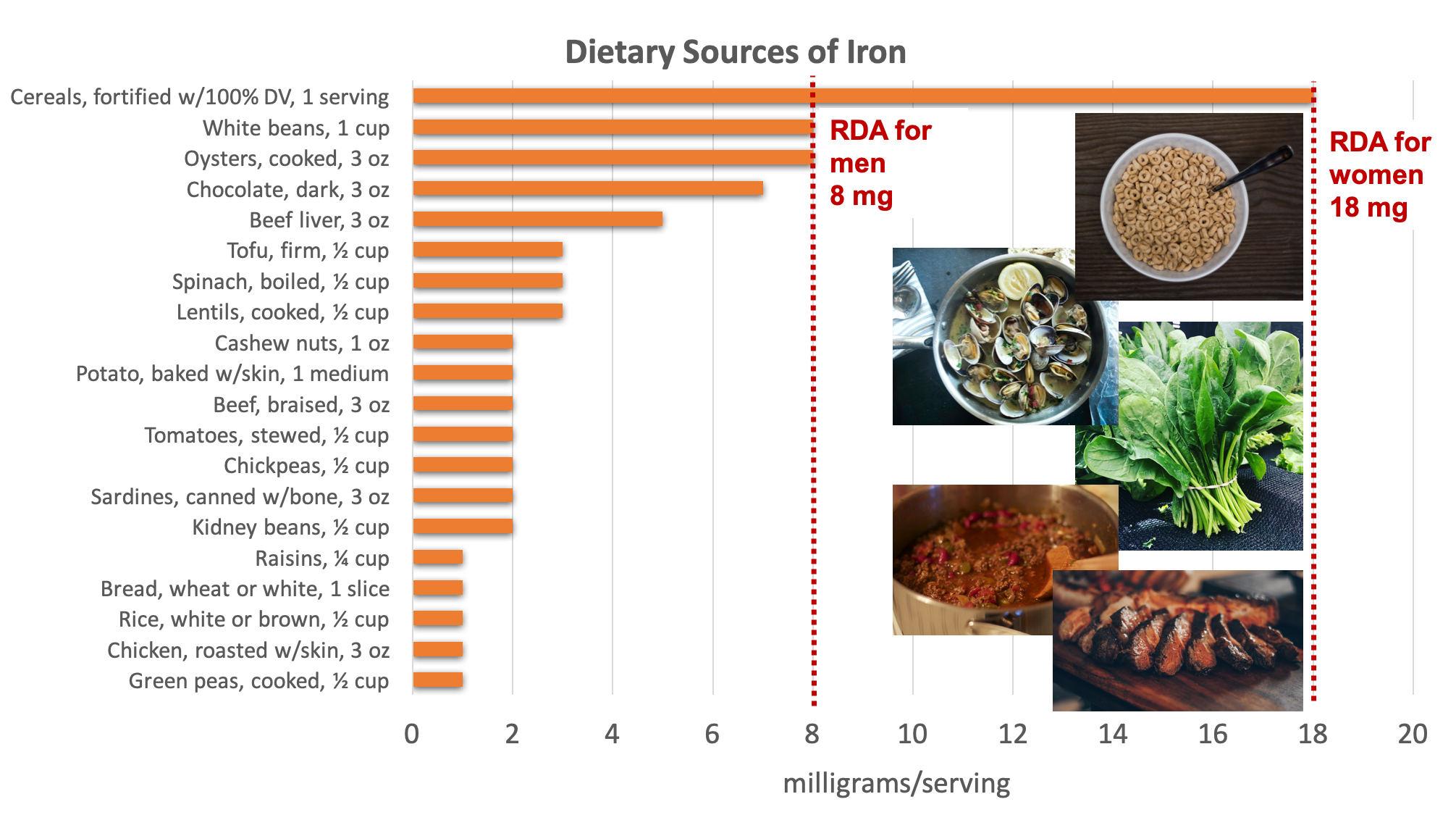
Figure 9.20. Dietary sources of iron. Examples of good sources pictured include fortified cereal, clams, spinach, lentils and red meat. Source: NIH Office of Dietary Supplements
The bioavailability of iron is approximately 14% to 18% from mixed diets and 5% to 12% from vegetarian diets.2 Bioavailability is influenced by the dietary factors previously mentioned, as well as iron status. The body has no physiological mechanism to excrete iron; therefore, iron balance is tightly regulated by absorption.2 When iron stores are low, more dietary iron will be absorbed.
The majority of the body’s iron needs are not met by dietary sources, but rather by recycling iron within the body (endogenous sources). Ninety percent of daily iron needs are met by recycling iron released from the breakdown of aging cells, mostly red blood cells.2
Iron Deficiency and Toxicity
Iron deficiency is one of the most common nutrient deficiencies, affecting more than a third of the world’s population.3 Iron-deficiency anemia is a condition that develops from having insufficient iron levels in the body, resulting in fewer and smaller red blood cells that contain less hemoglobin. As a result, blood carries less oxygen from the lungs to cells. Iron-deficiency anemia has the following signs and symptoms, which are linked to the essential functions of iron in energy metabolism and blood health:
- Fatigue
- Weakness
- Pale skin
- Shortness of breath
- Dizziness
- Swollen, sore tongue
- Abnormal heart rate
Infants, children, adolescents, and women are the populations most at risk worldwide for iron-deficiency anemia.4 Infants who are premature, low birthweight, or have a mother with iron deficiency are at risk for iron deficiency, because they are born with low iron stores relative to the amount needed for growth and development. Young children and adolescent girls are at risk for iron deficiency due to rapid growth, low dietary intake of iron, as well as heavy menstruation for adolescent girls. In these populations, iron-deficiency anemia can also cause the following signs and symptoms: pica (an intense craving for and ingestion of non-food items such as paper, dirt, or clay), poor growth, failure to thrive, and poor performance in school, as well as mental, motor, and behavioral disorders. Women who experience heavy menstrual bleeding, or who are pregnant, are also at risk for iron inadequacy due to their increased requirements for iron.
To give you a better understanding of these risks, it is helpful to look at how much higher the RDA is for women of reproductive age and pregnant women compared to men (Table 9.2).1 To put this in perspective, 3 ounces of beef contains about 3 milligrams of iron, making it challenging for some women to meet their daily iron requirement.
|
Population Group |
RDA for Iron |
|
Women of reproductive age, 19-50 years |
18 mg/day |
|
Pregnancy, 19- 50 years |
27 mg/day |
|
Men, 19-50 years |
8 mg/day |
Table 9.2. A comparison of the RDAs for adult women of reproductive age, pregnancy, and adult men.
Additionally, those who frequently donate blood, as well as people with cancer, heart failure, or gastrointestinal diseases such as Crohn’s, are at greater risk for iron inadequacy.1
Iron deficiency progresses through three stages:1
- Mild depletion of iron stores – No physical symptoms will be present, because hemoglobin levels are not affected, but there will be a decrease in ferritin (a storage form of iron).
- Iron-deficient erythropoiesis (erythrocyte or red blood cell production) – Iron stores are depleted and iron transport is decreased due to a decrease in transferrin (the transport protein for iron), but hemoglobin levels are usually within the normal range.
- Iron-deficiency anemia – Iron stores are exhausted and hemoglobin levels are reduced, resulting in microcytic anemia (small red blood cells) and hypochromic anemia (low color red blood cells).
Healthy adults are at little risk of iron overload from foods, but too much iron from supplements can result in gastric upset, constipation, nausea, vomiting, and abdominal pain.1 The body excretes little iron; therefore, the potential for toxicity from supplements is a concern. In children, death has occurred from ingesting as little as 200 mg of iron, so it is critical to keep iron supplements out of children’s reach. The tolerable upper intake for iron is 45 mg per day for adults, based on the amount that causes gastrointestinal distress.1
Vitamin K
Vitamin K refers to a group of fat-soluble vitamins that are similar in chemical structure. They act as coenzymes and have long been known to play an essential role in blood coagulation or clotting. Vitamin K is also required for maintaining bone health, as it modifies a protein which is involved in the bone remodeling process.
Dietary Sources of Vitamin K
Vitamin K is found in the highest concentrations in green vegetables such as collard and turnip greens, kale, broccoli, and spinach. Soybean and canola oil are also common sources of vitamin K in the U.S. diet.5 Additionally, vitamin K can be synthesized by bacteria in the large intestine, but the bioavailability of bacterial vitamin K is unclear.
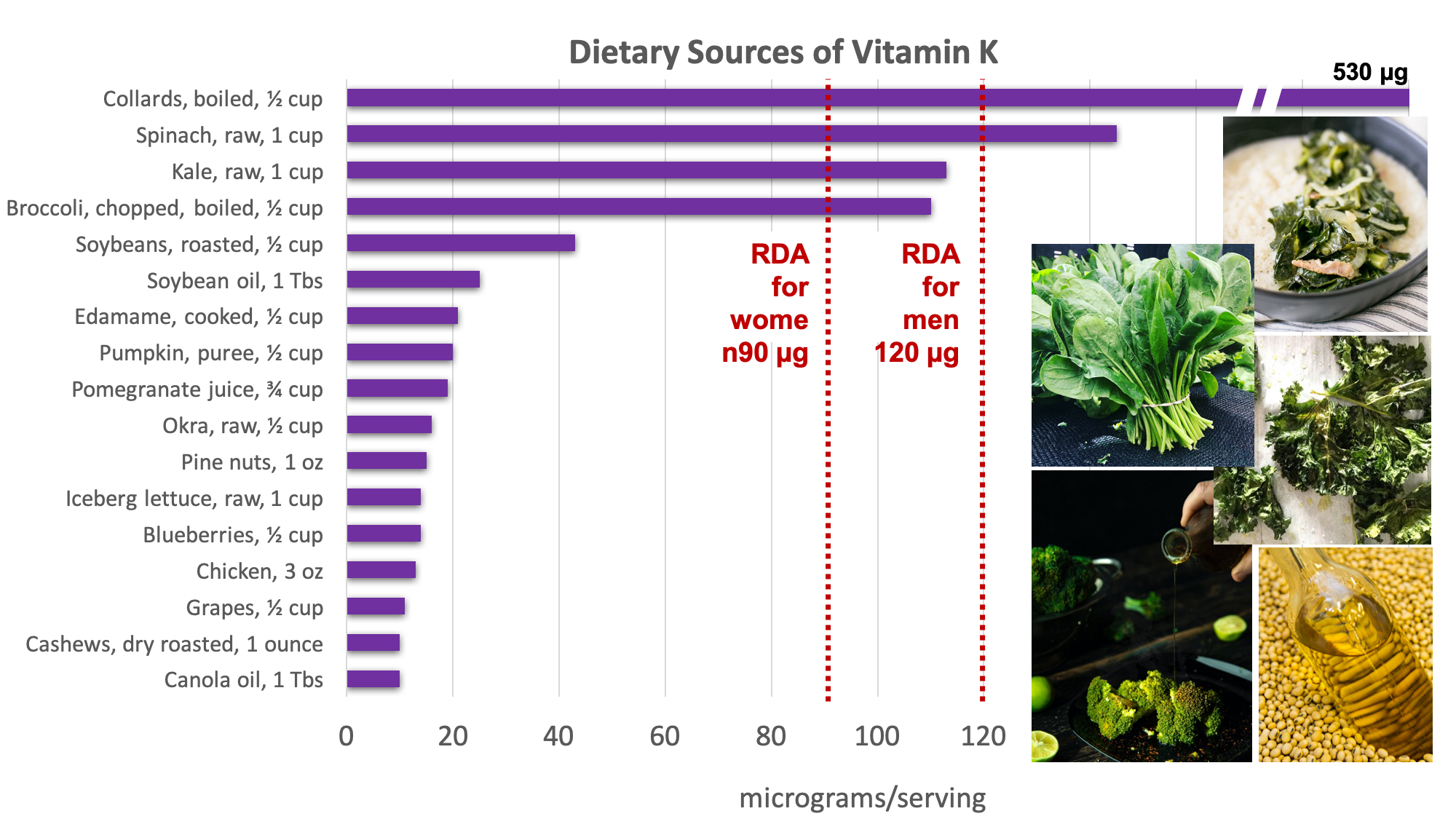
Figure 9.21. Dietary sources of vitamin K. Examples of good sources pictured include chard, spinach, kale, broccoli, and soybean oil. Source: NIH Office of Dietary Supplements
Vitamin K Deficiency and Toxicity
Vitamin K deficiency is rare, as most U.S. diets are adequate in vitamin K.5 A deficiency in vitamin K causes excessive bleeding (or hemorrhage). When there is damage to a blood vessel that results in bleeding, like a small tear, the body can stop this bleeding through a cascade of reactions. Without adequate vitamin K, blood does not clot properly, and this small bleed can turn into a larger problem, causing excessive bleeding or hemorrhage. People at risk are those who have malabsorption and other gastrointestinal disorders such as celiac disease. Newborns are also at risk for vitamin K deficiency during the first few months of life, as there is poor transfer of vitamin K across the placenta, and breastmilk is also low in vitamin K. Therefore, it has become a routine practice to inject newborns with a single intramuscular dose of vitamin K to prevent hemorrhaging, as bleeding within the skull is especially life-threatening.
The Food and Nutrition Board (FNB) has not established a UL for vitamin K because it has a low potential for toxicity.
Self-Check:
Attributions:
- Zimmerman, M., & Snow, B. Blood’s Function in the Body and in Metabolism Support. In An Introduction to Nutrition (v. 1.0). https://2012books.lardbucket.org/books/an-introduction-to-nutrition/index.html, CC BY-NC-SA 3.0
- Lindshield, B. L. Iron Deficiency and Toxicity. Kansas State University Human Nutrition (FNDH 400) Flexbook (2018). NPP eBooks. 19. http://newprairiepress.org/ebooks/19 CC BY-NC-SA 4.0
Resources:
- 1National Institutes of Health of Dietary Supplements. Iron – Health Professional Fact Sheet. Retrieved April 29, 2020 from https://ods.od.nih.gov/factsheets/Iron-HealthProfessional/
- 2Richard Hurrell, Ines Egli, Iron bioavailability and dietary reference values, The American Journal of Clinical Nutrition, Volume 91, Issue 5, May 2010, Pages 1461S–1467S, https://doi.org/10.3945/ajcn.2010.28674F
- 3Chaparro, C. M., & Suchdev, P. S. (2019). Anemia epidemiology, pathophysiology, and etiology in low- and middle-income countries. Annals of the New York Academy of Sciences, 1450(1), 15–31. https://doi.org/10.1111/nyas.14092
- 4Powers JM, Buchanan GR. (2019). Disorders of iron metabolism: New diagnostic and treatment approaches to iron deficiency. Hematol Oncol Clin North Am, 33(3):393-408, doi: 10.1016/j.hoc.2019.01.006
- 5National Institutes of Health of Dietary Supplements. Vitamin K – Health Professional Fact Sheet. Retrieved April 29, 2020 from https://ods.od.nih.gov/factsheets/VitaminK-HealthProfessional/
Images:
- Figure 9.18. “Structure of Hemoglobin” by Zephyris at English Wikipedia is licensed under CC BY-SA 3.0 and “Heme” by Yikrazuul is in the Public Domain
- Table 9.2. “A comparison of the RDAs” by Tamberly Powell is licensed under CC BY 4.0 with data from National Institutes of Health of Dietary Supplements. Iron – Health Professional Fact Sheet. Retrieved April 29, 2020 from https://ods.od.nih.gov/factsheets/Iron-HealthProfessional/#en4
- Figure 9.19. “Dietary sources of iron” by Alice Callahan is licensed under CC BY 4.0, with images: Breakfast cereal by John Matychuk, clams by Adrien Sala, spinach by Elianna Friedman, steak by Emerson Vieira on Unsplash (license information); “Superbowl Chili” by Jake Przespo is licensed under CC BY 2.0.
- Figure 9.20. “Dietary sources of vitamin K” by Alice Callahan is licensed under CC BY 4.0, with images: Collards by Kim Daniels, spinach by Elianna Friedman, kale by Ronit Shaked, broccoli by Hessam Hojati, all on Unsplash (license information); “High oleic acid soybean oil_0030” by Mizzou CAFNR is licensed under CC BY-NC 2.0
Also known as erythrocytes; transport oxygen to cells and remove carbon dioxide from cells.
Also known as leukocytes; immune cells that help destroy foreign invaders.
Fragments of cells that circulate and assist in blood clotting.
The fluid component of the blood.
A protein in red blood cells that transports oxygen to cells and gives red blood cells their color.
A condition in which oxygen-carrying capacity of red blood cells is reduced, often from a reduction in hemoglobin.
A protein similar to hemoglobin but found in muscles; provides oxygen to muscles.
Iron that is part of the proteins hemoglobin and myoglobin; most bioavailable form of iron, found only in animal foods.
The mineral form of iron by itself, not a part of hemoglobin or myoglobin; found in foods from both plants and animals and is less bioavailable than heme iron.
A condition that develops from having insufficient iron levels in the body, resulting in fewer and smaller red blood cells that contain less hemoglobin.
An intense craving for and ingestion of non-food items such as paper, dirt, or clay.
A storage form of iron.
The transport protein for iron.
A type of anemia characterized by small red blood cells.
A type of anemia characterized by low color red blood cells.
Also known as clotting; the process by which blood changes from a liquid to a semi-liquid or gel to form a clot.
Excessive bleeding.

