7.2 Health as a Social Problem

Figure 7.3 Medical providers must use universal precautions such as masks and gloves when treating patients with communicable diseases such as Ebola and COVID-19.
Even with our brief explanation of COVID-19 statistics in the introduction of this chapter, we see that people experience unequal health outcomes based on their race and ethnicity. This is just one dimension of inequality in health outcomes. What else makes health and illness a social problem?
Health and illness in society go beyond individual experience. We usually think of health, illness, and medicine in individual terms. When a person becomes ill, we view the illness as a medical problem with biological causes. A physician treats the individual accordingly. A sociological approach takes a different view. Unlike physicians, sociologists and other public health scholars do not try to understand why any one person becomes ill. Instead, we typically examine rates of illness to explain why people from certain social backgrounds are more likely than those from others to become sick. Our social location in society—our social class, race and ethnicity, gender, and other dimensions of difference—makes a critical difference.
Medical sociology is the systematic study of how societies manage issues of health and illness, such as diseases and disorders, healthcare access, as well as the larger picture of physical, mental, and social components of health and illness. Major topics for medical sociologists include the doctor/patient relationship, the structure and socioeconomics of healthcare, and how culture impacts attitudes toward disease and wellness. In the next section, we’ll look at what medical sociologists find when they look at how experiences of health and illness can differ by social location.
How we get sick and how we stay healthy reveal our interdependence. As an example, residents of Flint, Michigan, experienced higher than normal levels of lead toxicity, hair loss, rash, and other health issues when the local municipal government changed the water supply in 2013. Although government officials knew that the Flint River was contaminated with pollution from manufacturing, they decided to use this water for city residents because it was cheaper. Decisions at several interdependent layers of government resulted in this harmful decision. Local citizens connected with doctors, health officials, and journalists to tell the story of the contaminated water and support a change. Eventually, the Michigan Civil Rights Commission cited systemic racism as the fundamental cause for the questionable decisions. Recovery required both individual agency and collective action. If you would like to learn more, Flint Water Crisis: Everything You Need to Know provides more details.
Conflict between values can cause social problems to arise. How would you describe the difference in values between the social groups represented in figures 7.4 and 7.5?
Figure 7.4 Pandemic lockdown protesters hold signs that say that lockdown is an issue of tyranny and freedom.
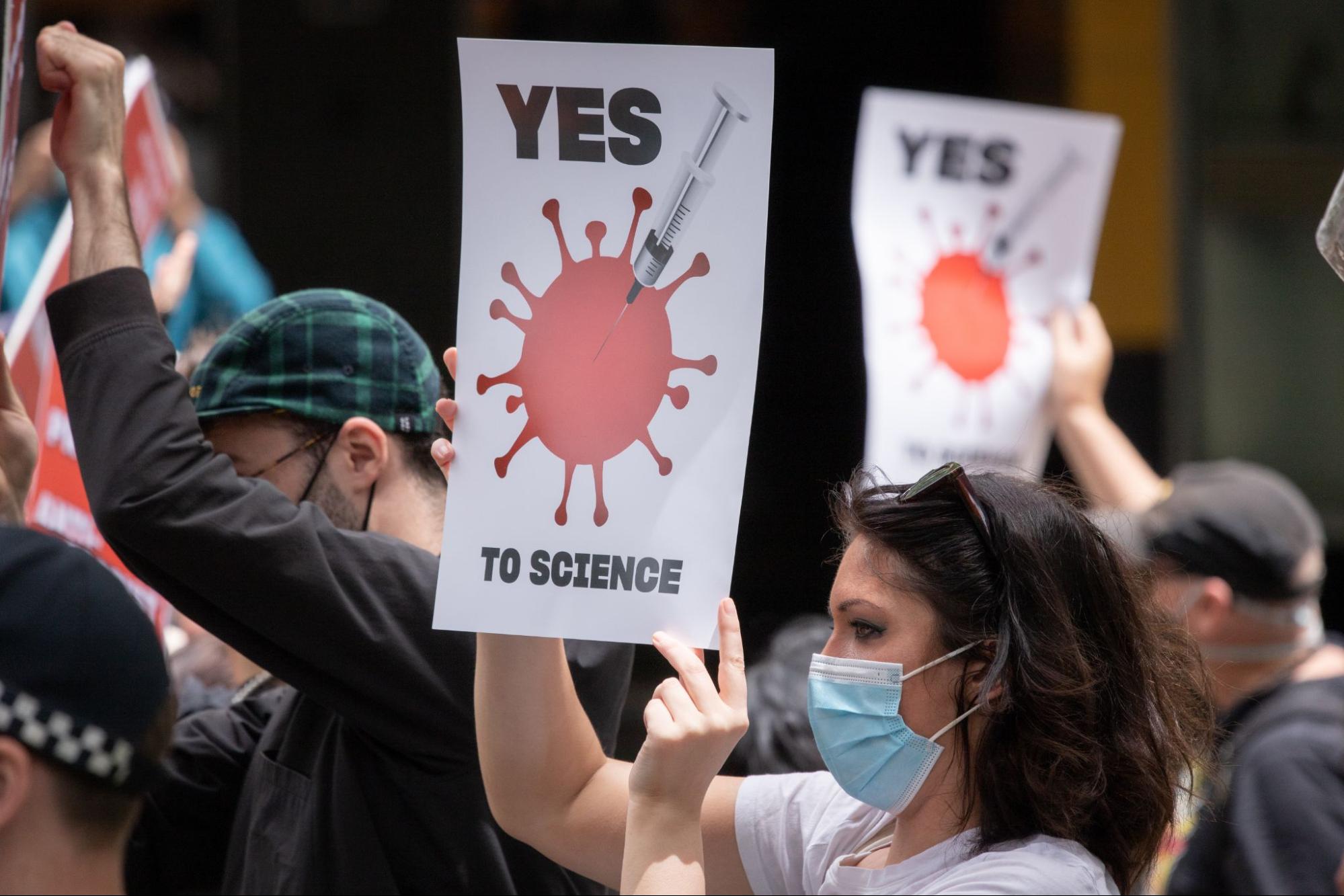
Figure 7.5 Pandemic protesters hold signs that promote using science to end the pandemic.
The protesters in figure 7.4 explicitly state that the COVID-19 lockdown is an example of government tyranny. The protesters in figure 7.5 are promoting vaccinations, asserting that scientific knowledge and research should be used to ensure our health. You may know people who support vaccines and social distancing as a way to manage the pandemic. You may know other people who think that vaccines are dangerous and that state-mandated quarantining is “un-American.” This conflict in values creates the conditions in which a social problem is likely to arise.
Many conversations on social media in the United States focused on a perceived loss of personal freedoms caused by quarantining, social distancing, and wearing face coverings. Dr. Anthony Fauci, the Director of the National Institute of Allergy and Infectious Diseases and the Chief Medical Advisor to the President, became a symbol of strength for those supporting vaccination and following guidelines, while at the same time becoming the feature of many t-shirts and bumper stickers for those who were critical of the federal government’s implementation of World Health Organization (WHO) guidelines for reducing the spread of COVID-19.
Our ideas about what is healthy, what is illness, and what actions we should take to be healthy and treat illness, are socially constructed. The fact that our social backgrounds affect our health may be difficult for many of us to accept. We all know someone, and often someone we love, who has died from a serious illness or currently suffers from one. There is usually a physical or biological cause of this person’s illness, and physicians do their best to try to cure it and prevent it from recurring. Sometimes they succeed; sometimes they fail. Whether someone suffers a serious illness is often a combination of life events and the biological traits that we inherit from our parents (Cockerham 2009). The exact details of how one’s social, cultural, ethnic, and genetic profile impact your health and likelihood of contracting diseases is a rapidly evolving research area. The study of how our behaviors and environment can cause changes that affect the way our genes work is called epigenetics. The medical and sociology communities are not shy in sharing that our social backgrounds affect our health, but many genetic studies erroneously correlate health outcomes with racial identity.
A sociological approach also emphasizes that a society’s culture shapes its understanding of health and illness and practices of medicine. In particular, culture shapes a society’s perceptions of what it means to be healthy or ill, the reasons to which it attributes illness, and the ways in which it tries to keep its members healthy and cure those who are sick (Hahn & Inborn 2009). Knowing about a society’s culture, then, helps us to understand how it perceives health and healing. By the same token, knowing about a society’s health and medicine helps us to understand important aspects of its culture. We’ll look more deeply into cultural constructions of health and illness in section 7.4.
We can also look at health and illness through the lens of the social problems process, using COVID-19 as an example. As we discussed in Chapter 1, the social problems process is a model to explain social phenomena and predict what might happen next. The response to COVID-19 is an unusual example because government action was often the first step in response to a social problem, rather than the more common starting places of protest and activism. We start our cycle then at Step 4: Policymaking. Governments worldwide responded to the pandemic differently, resulting in a variety of social consequences.
While some countries managed the spread of the virus far better than others, it affected everyone. Highly industrialized countries, such as China, Italy, and the United States, were early centers of the outbreak. Brazil and India had later increases, as did the U.K. and Russia. Most countries took measures that were considered extreme by Americans—closing borders, forcing schools and businesses to close, and requiring face coverings to be worn when leaving one’s home. Other nations went further, completely shutting down at the discovery of just a few cases. And some countries had mixed responses, typically resulting in high rates of infection and overwhelming losses of life. In Brazil and the United States, for example, political leaders and large swaths of the population rejected measures to contain the virus. By the time vaccines became widely available, those two countries had the highest numbers of COVID-19 deaths worldwide.
Prior to the United States facing the worst COVID-19 outbreak in the world, the federal government restricted travel, as did many countries in Europe. Shutting down travel, instituting social distancing, and closing down schools were examples of Step 5 Social Problems work, the creation of actual practices and behaviors that implement government policies.
With the implementation of these policies, we begin to see Step 6, Policy Outcomes. Government action was focused on “flattening the curve,” or decreasing the amount of people who needed hospitalization at any one time. We continue to measure and report the outcomes of these policies and will continue to interpret them.
In the meantime, the cycle continues. We see new claims being made, Step 1, and the related media coverage of those claims, Step 2. Conflicting messages about mask wearing and social distancing became political weapons amid the country’s 2020 Presidential election, and localized outbreaks and spikes of deaths were continually traced to gatherings that occurred against scientific guidance. Brazil’s President actively disputed medical opinions, rejected any travel or business restrictions, and was in conflict with many people in his own government (even his political allies). With Brazil’s slower pace of vaccination compared to the U.S., it saw a steep increase in cases and deaths just as the United States’ numbers started to decline.
Both those opposed to heavy restrictions and those who used them to fight the disease acknowledge that the impacts went far beyond physical health. Families shattered by the loss of a loved one had to go through the pain without relatives to support them at funerals or other gatherings. Many who recovered from the disease had serious health issues to contend with, while other people who were forced to delay important surgical and other medical treatments faced financial, emotional, and mental health challenges because of COVID-19 restrictions implemented at all levels of government. Fear, isolation, and strained familial relationships led to emotional problems. Many families lost income. Learning was certainly impacted as educational practices went through sudden shifts. The true outcomes will likely not be fully understood for years after the pandemic is under control.
So now, after the height of the COVID-19 pandemic, what does health mean to you? Does your opinion of it differ from your pre-COVID attitudes? Many people who became severely ill or died from COVID had other health issues such as hypertension and obesity. Do you know people whose attitudes about their general health changed? Do you know people who find themselves suspicious of the intentions of the government, or less likely to listen to doctors or scientists? What do you think will be the best way to prevent illness and death should another pandemic strike? Each of these questions highlights a topic related to the social construction of the social problem of health and illness.
7.2.1 Licenses and Attributions for Health as a Social Problem
“Health as a Social Problem” by Kate Burrows and Kim Puttman is licensed under CC BY 4.0.
New social problems content remixed with Introduction to Sociology 3e 19 Introduction and 19.1 The Social Contruction of Health CC-BY-4.0 and Sociology: Understanding and Changing the Social world 18.1 Understanding Health Medicine and Society Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License,
Figure 7.3 Navy Medicine/flickr from https://openstax.org/books/introduction-sociology-3e/pages/19-introduction
Figure 7.4 An anti-lockdown protest at Queen’s Pa… | Flickr
Figure 7.5 Yes to Science protesters Photo by Mitchell Luo on Unsplash
