7.1 Chapter Overview
My deepest gratitude goes to Kim Puttman, who helped guide me as I wrote this chapter during a tumultuous period of my life. She was a thoughtful tutor and mentor, and this chapter wouldn’t have been written without her. – Kate Burrows
Figure 7.1 Isaiah – Voices of Long COVID [YouTube Video] and Inside a long Covid clinic: ’I look normal, but my body is breaking down’ [YouTube Video]. These two videos tell the story of people with long haul COVID-19. As you watch, please consider how these experiences might create a social problem. Opening Question: How did you and your family experience COVID-19?
By now, we probably all can tell a story about how COVID-19 has impacted our lives. Some of us have had family members or friends pass away. Some of us are still experiencing lingering symptoms from a COVID-19 infection (called long-haul or long COVID, figure 7.1). Some of our kids just felt achy or tired for a day and then got better. Some of us may not know anyone who was personally affected by COVID-19. Pause for a moment to think about your own COVID-19 health story, and consider the many ways that this disease has affected society in the United States and worldwide .
My personal COVID-19 story has many layers. My wife and I quarantined, masked, and stayed socially distant for over two years. We isolated ourselves stringently because both of us have underlying health conditions which would make surviving COVID-19 difficult. My four parents followed these same protocols, missing visits with grandchildren, graduations, and family holidays. My dad had his 80th birthday party on Zoom, an event that we never could have predicted. My brothers and their families quarantined as requested early in the pandemic. They attended school from home, just as many governors ordered. One sister-in-law still went to the hospital to deliver babies and care for patients sick with COVID-19.
Luckily, no one in my close family had to be hospitalized for COVID-19, and no one passed away. People in my close family got sick, but everyone has recovered. Luck might have kept my family well, but equally important to consider is my social location. My family had safe, warm, comfortable housing where we could quarantine. We could order food and supplies online, and people would deliver them to our door. Many of us were able to complete our work remotely, or at least adjust our work schedules. Although we had to wait until our age groups were eligible, our family had relatively easy access to vaccines. While these advantages don’t guarantee health, they gave us options to respond effectively during the pandemic.
This story highlights how health itself becomes a social problem, not just a medical one. Common sense tells us that since COVID-19 is a disease, it should affect all people equally. You would think that a virus wouldn’t discriminate.
However, we have learned that some social groups are more likely to be infected, hospitalized, and even die as a result of contracting COVID-19. The table in figure 7.2 shows rates of cases, hospitalizations, and deaths due to COVID-19 by race and ethnicity. As you can see, non-Hispanic Black people die from COVID-19 at a rate twice that of White people. Please take a moment to look at the other differences related to race and ethnicity in this table.
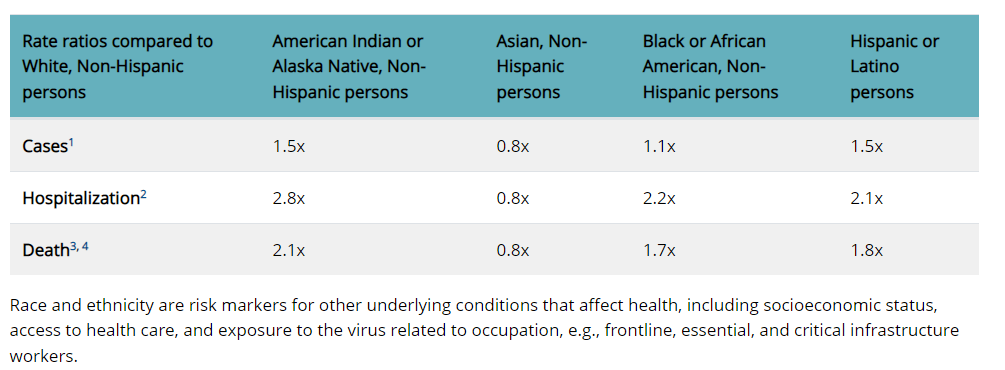
Figure 7.2: Rates for COVID-19 Infection, Hospitalization and Death y Race/Ethnicity, as of July 28, 2020. Race and ethnicity are risk markers for other underlying conditions that affect health, including socioeconomic status, access to health care, and exposure to related occupations, e.g. frontline, essential and critical infrastructure workers, Figure 7.2 Image Description
Perhaps you notice that the data show a gap between European Americans and American Indian/Alaskan Native, Asian, Black people, and Latinx people. As you can see in the table, cases, hospitalizations, and deaths for all ethnic groups except for Asians are substantially higher than for Whites. This experience of inequality demonstrates that health and illness can be social problems.
In this chapter, we will explore the social elements of health, a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity. We will look more deeply at why health is a social problem. We will look at how sociologists make sense of health and illness by considering how these understandings develop over time. We will explore collective and individual models of the social determinants of health. As we deepen our understanding of the social determinants of health, we will include the experience of individual and generational trauma as a factor in health outcomes. Like many other social problems, government policies and practices influence access to health resources and health outcomes. We will look at the differences in health systems internationally, and decide if these systemic differences support health for everyone. Finally, we will come back to our own COVID-19 stories. The pandemic has both exposed and worsened existing inequalities. The pandemic is also inspiring creative action from individuals, communities, and governments. These generous responses demonstrate our interdependence.
7.1.1 Focusing Questions
The questions that encourage our curiosity include:
- How is health a social problem?
- How do sociologists make sense of health and illness? How have our definitions changed over time?
- What are social determinants of health, and how do they influence health outcomes for individuals and communities?
- In what ways do social values and government policies impact health systems and health outcomes in the U.S. and worldwide?
- How has COVID-19 provided an opportunity to assess and improve healthcare delivery and health outcomes?
Let’s get started!
7.1.2 Licenses and Attributions for Chapter Overview
“Chapter Overview” by Kate Burrows and Kim Puttman is licensed under CC BY 4.0.
Figure 7.1 a “Anyone can get Long COVID:Isaiah” © Resolve to Save Lives. License Terms: Standard YouTube License.
Figure 7.1 a “Inside a Long Covid clinic: “I look normal, but my body is breaking down”” © The Guardian. .License Terms: Standard YouTube License.
Figure 7.2: Risk for COVID-19 Infection, Hospitalization, and Death By Race/Ethnicity Center for Disease Control (CDC). Public Domain
