5 Histology of glands, lymphatics and sinuses
- Basic anatomy
- Salivary glands
- Components of saliva
- Dental pellicle
- Histology of salivary glands
- Anatomy of salivary glands
- Clinical applications of gland histology
- Lymphatic system
- Lymph nodes
- Tonsils
- Clinical application of lymphatic histology
- Sinuses
- Para-nasal sinus anatomy
- Clinical application of para-nasal sinus histology
Basic anatomy of exocrine glands and lymphatic organs
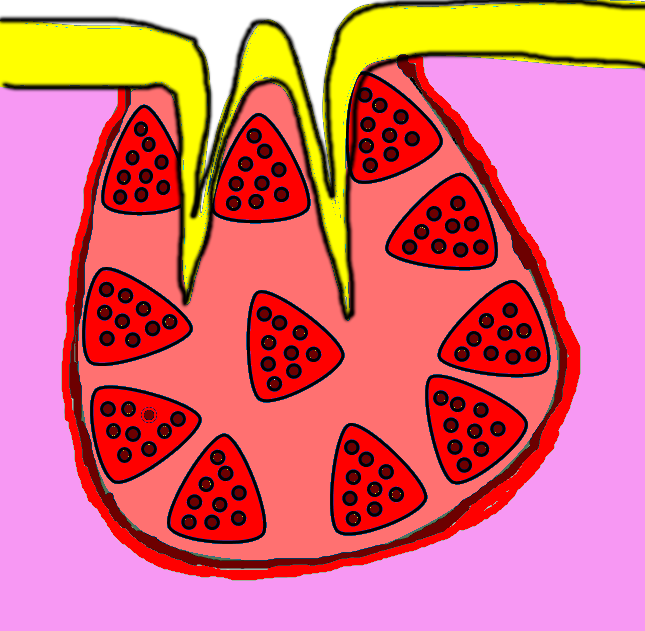
The average exocrine gland contains simple cuboidal epithelia← that form grape-shaped or tube-shaped structures called acini. Liquids secreted by the cells of acini enter a duct, which can be made of a simple cuboidal epithelium or simple columnar epithelium←. It is possible for larger glands to have regions of stratified cuboidal epithelial cells as well. The outside of the gland is surrounded by a dense connective tissue capsule (not quite thick enough for us to worry about whether the collagen← fibers are regular or irregular). The connective tissue extends inwards forming trabeculae (or septa, but not to be confused with trabeculae of spongy bone tissue), which divide the organ into lobes.
The average lymphatic organ shares patterns with exocrine glands. A lymphatic organ is surrounded by a dense connective tissue capsule, and that connective tissue extends inwards forming trabeculae. Inside a lymphatic organ, clusters of white blood cells suspended within reticular connective tissue form germinal centers (or nodules) where white blood cells filter cellular debris and scan body fluids for pathogens. If they detect a pathogen, they multiply, release inflammatory signals, and migrate through the body’s connective tissues looking for more pathogens.
Salivary glands

"Suspected meth mouth" by Dozenist, is licensed CC BY SA 3.0Components of saliva
The major function of salivary glands is to produce saliva, which helps maintain the health of the oral mucosa and teeth, as well as assist in mastication. Acinar epithelial cells transcribe and translate long mucous proteins on the rER←, modify them in the Golgi apparatus← to form large glycoproteins, and secrete them. These cells also pump electrolytes from their cytoplasm into the lumen of the acinus, which, along with the glycoproteins, attract water by osmosis. These components make saliva moist but sticky enough to adhere to all surfaces of the oral cavity, rather than sink to the floor of the mouth.
Other molecules are secreted and become a part of saliva. Buffers within saliva help to maintain a stable pH, despite the acidity or alkalinity of different foods, or the acidity of certain oral bacterial secretions. Buffers and electrolytes also help disrupt the formation of bacterial biofilms, which bacteria use to adhere to teeth. The watery nature of saliva helps to moisten food and the oral mucosa, assisting in mastication, speech and swallowing. Watery saliva also helps to limit the population of oral bacteria. People swallow saliva even when they are not eating. This flushes a percentage of oral microorganisms down to the stomach, where certain death awaits in the form of hydrochloric acid and the protein-destroying enzyme pepsin. The enzymes salivary amylase and lysozyme are produced by acinar cells to serve a similar purpose, breaking covalent bonds within the cell walls of viruses and bacteria, or their surface glycoproteins used to adhere to tooth surfaces. Without hours of mechanical digestion by the teeth and stomach, there is very little surface area for salivary amylase to digest carbohydrate molecules for nutritional purposes. Chemical digestion of carbohydrates for nutrition is carried out in the small intestines by the much more abundant pancreatic amylase. Bacteria, however, do not form a bolus (a large solid mass), so their cell walls and surface glycoproteins are open to attack by enzymes without prior mechanical processing. A second function of salivary amylase is to cleave a small amount of small sugars from starch, allowing taste buds to detect them, so salivary amylase and other carbohydrases in saliva function in the sense of gustation as well as in limiting bacterial populations.
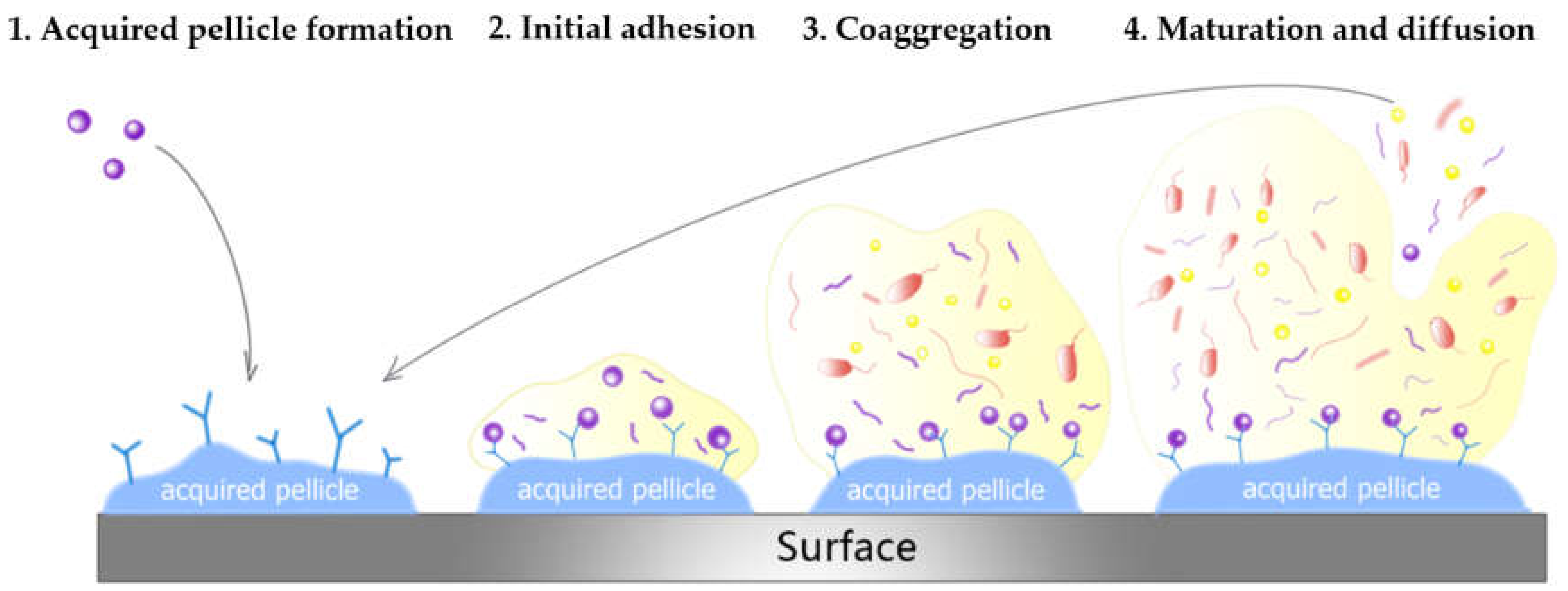
Dental pellicle
The dental pellicle is a thin coating of glycoproteins from saliva on the surface of teeth. It prevents excess deposits of Ca2+PO43- (calculus deposit minerals) and also prevents demineralization of enamel. Both depositing bumps or eroding crevices allows bacteria to adhere to teeth and avoid being washed into the stomach. Therefore, the dental pellicle can prevent adhesion of bacteria to the tooth surface. However, oral bacteria can adhere to the dental pellicle. Furthermore, saliva contains minerals that produce calculus, making the relationship between saliva, dental pellicle and the oral microbiome complicated. This illustrates the delicate balance that must be maintained in the oral cavity: too many bacteria can lead to gingivitis← and dental caries, while too few bacteria leave the oral cavity open to colonization by harmful bacteria, leading to gingivitis and dental caries.
Histology of salivary glands
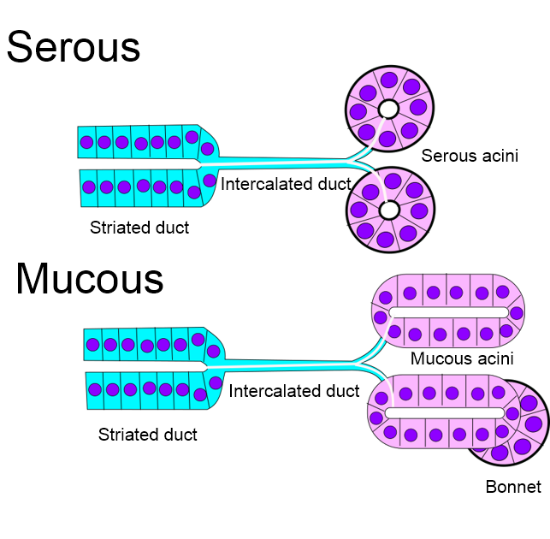
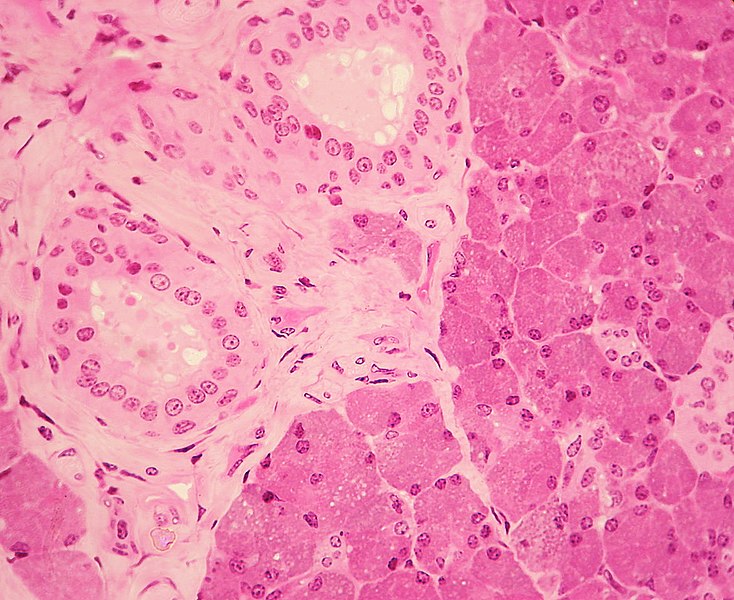
"Stratified cuboidal/columnar epithelium is visible in a duct surrounded by connective tissue in the parotid gland" by Wbensmith is licensed under CC BY 3.0Serous acini produce more watery secretions. These are composed of simple cuboidal epithelium←. Serous acini tend to stain darker pink or purple using a traditional H&E stain.
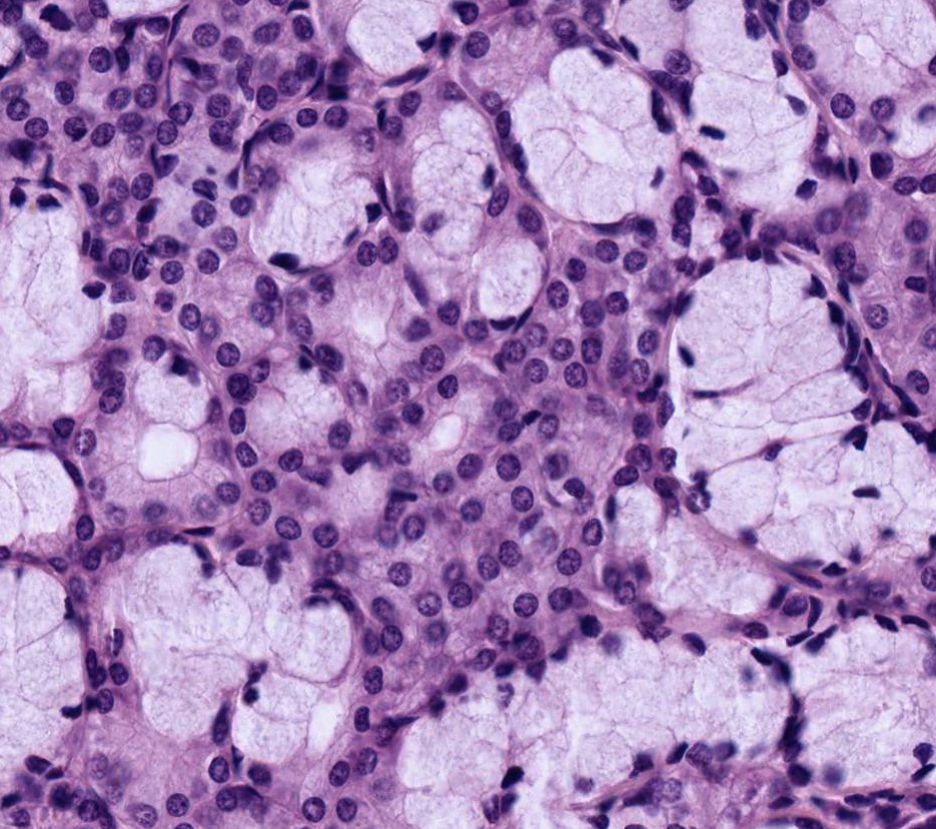
"major salivary glands" by Dr. Patrice Spitalnik, Columbia University Center for Teaching and Learning is licensed under CC BY-SA 4.0Mucous acini secrete more glycoproteins, making their secretion thicker and stickier (more mucous). Mucous acini are made of a simple columnar epithelium←. Mucous acini appear to have bubbles.
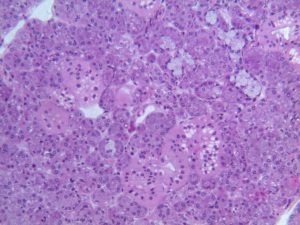
Muco-serous acini produce secretions halfway in-between the first two in consistency. These look like mucous acini under the microscope, with an additional bonnet (a hat) of myo-epithelial cells. These cells contract like smooth muscle cells. For most epithelial cells, the actin and myosin genes are found in the cytoskeleton← and allow for migration, which is especially important for stem cells← that move to help repair a wound. Myo-epithelial cells, on the other hand, use some of the DNA instructions for making larger amounts of actin and myosin and organizing them into specialized filaments similar to smooth muscle tissue. This makes myo-epithelial cells appear more like smooth muscle than an epithelium. However, these cells have an epithelial lineage— they differentiate← from ectoderm, not from a mesenchymal stem cell or myoblast.
All three secretions mix in the oral cavity to produce saliva. These secretions reach the oral cavity by way of different ducts, which can be identified under the microscope by their different types of epithelial cells. We know of no clinical significance to the types of ducts or their cells.
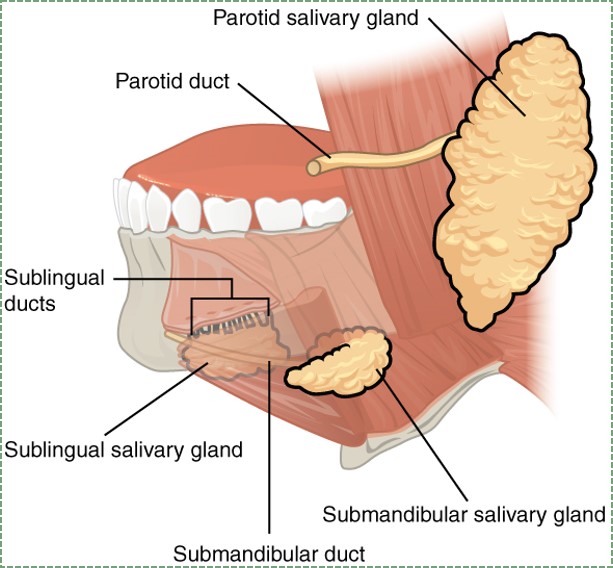
"Salivary glands" by OpenStax college, is licensed CC BY 3.0Anatomy of exocrine glands
There are three major and numerous minor salivary glands. The three major salivary glands are listed in Table 5.1.
| Major salivary gland | Details |
|---|---|
| Parotid salivary glands | Largest |
| Serous (mostly) | |
| 25% saliva by volume | |
| Sub-mandibular salivary glands | 2nd largest |
| Muco-serous | |
| 65% saliva by volume | |
| Sub-lingual salivary gland | Mucous |
| 10% saliva by volume |
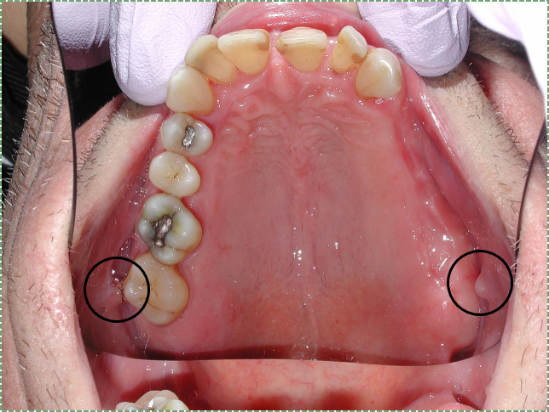
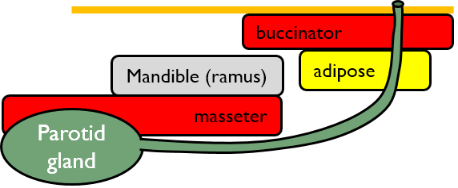
"Parotid duct papillae" by D Rosenbach, is licensed CC BY SA 3.0The parotid glands drain into the oral cavity by way of the parotid duct (or Stensen duct). The ducts travel through the masseter muscle and enters the oral cavity at a papilla on the buccal mucosa usually located lateral to the 2nd maxillary molar.
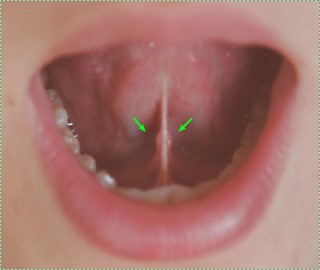
"Carruncula sublingularis" by Hellerhoff, is licensed CC BY SA 3.0The sub-lingual glands and sub-mandibular glands have ducts that share an entrance on the floor of the mouth at the sub-lingual caruncle. The sub-lingual gland also has numerous smaller ducts that open onto the floor of the mouth.

"Nicotinic stomatitis" by DVIDS is in the Public Domain CC0Numerous minor salivary glands are located throughout the oral cavity. They are normally not visible, unless the oral mucosa is hyper-keratinized. Luckily, no one has bothered to name these glands or their ducts, except for the von Ebner salivary glands, which are minor salivary glands associated with the circumvallate lingual papillae. The minor salivary glands are predominantly mucous, with exceptions, which helps their secretions to stick to the roof and sides of the oral cavity.
Clinical application of salivary gland histology
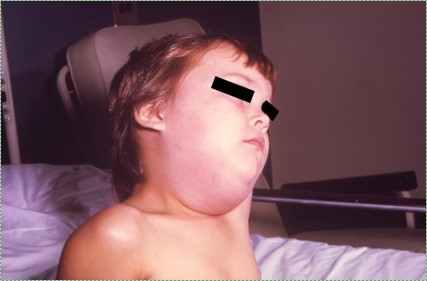
"Mumps" by Photo CDC/NIP/Barbara Rice, is in the Public Domain CC0Mumps is a viral infection that causes swelling of the parotid glands and other organs. Vaccination has reduced mumps cases in the US by over 99%. Vaccination against mumps works by triggering the primary immune response against mumps antigens. Unfortunately, mumps outbreaks still occur, often in high-density living areas (such as college dormitories) with a large percentage of unvaccinated individuals. It is difficult to counter beliefs in pseudoscience which seek to cast doubt on the safety or efficacy of vaccination, although some strategies work better than others.

"Angular cheilitis" by Matthew Ferguson, is licensed CC BY SA 3.0Hypo-salivation
Hypo-salivation, or decreased saliva production, can be caused by certain diseases, medications, cancer treatments, and aging. It may result in xerostomia, or dry mouth. Because saliva contains growth factors, reduced saliva decreases the healing ability of the oral mucosa, leading to sores. Reduced saliva also reduces limits to growth placed on the oral microbiome, leading to infections and caries. Reduced taste can also be a consequence, which patients might compensate for by flavoring their food with excessive levels of salt (NaCl). Using Monosodium Glutamate (MSG, or NaC5H8NO4) may be used to enhance both flavor and saliva production, and is a significantly healthier option.

"Salivary gland stone and the operation mark" by Peter Nickson, is in the Public Domain CC0Mineralized saliva (sialoliths)
Electrolytes in saliva can precipitate and form salivary gland stones, or sialoliths. Large sialoliths may block the duct of one of the salivary glands, which stops the flow– but not the production– of saliva. As a result, saliva builds up in the gland, causing swelling and possibly inflammation. Blockage of a minor salivary gland produces a swelling within the oral mucosa known as a mucocele (or mucocoele) (Fig. 5.14), while blockage of a major salivary gland produces a ranula (Fig. 5.15). These are fairly common disorders. Inflammation of the parotid gland must be clearly distinguished from mumps before any treatment is given.

"Mucocoele" by Dozenist is licensed CC BY SA 3.0
"Ranula" by Ph0t0happy is licensed CC BY SA 3.0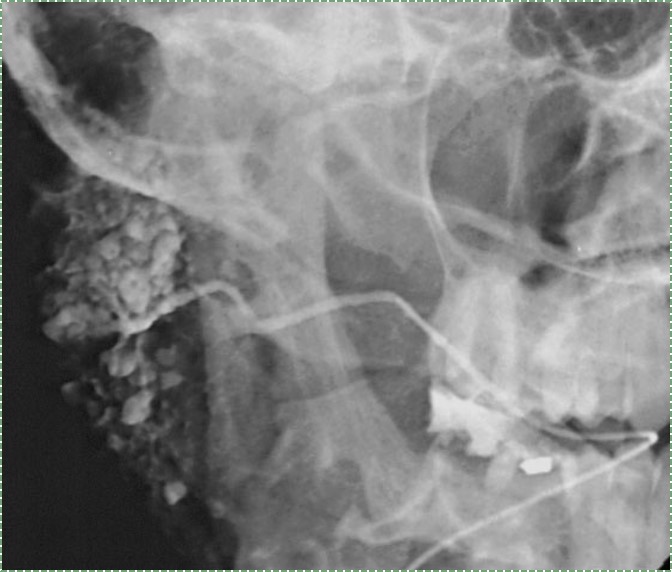
"Own work" by Hellerhoff, is in licensed CC BY SA 3.0Sialography
Sialoliths may be palpated by clinicians. Alternately, an image of the blockage known as a sialograph can be taken by injecting a radiopaque dye as far into the salivary gland duct as it can go (until further flow is blocked by the sialolith). Usually, sialoliths are removed with minimal discomfort. Sialography should not be done in cases of acute infection, as the dye may push infectious exudate into deeper tissues, spreading the infection.
Lymphatic system
Very basic overview of the lymphatic system
| Lymphatic organ | Major function |
|---|---|
| Lymphatic vessels | Drain ECF off organs, including teeth |
| Lymph nodes | Filter debris and identify pathogens |
| Tonsillar tissue | Identify pathogens |
| Other lymphatic organs | Located below the neck |
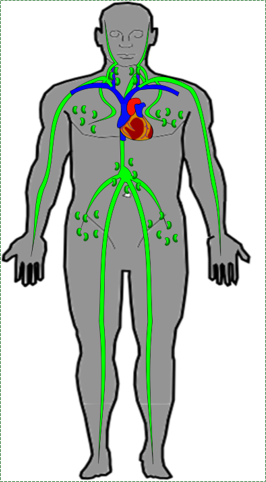
"Own work" by Goran tek-en, is licensed CC BY SA 3.0 / Arrows and animation addedLymphatic drainage of the teeth
Fluid travels to the teeth via capillaries. As plasma exudes from the capillaries, it becomes ECF. Veins collect most of this fluid, the rest is collected by lymphatic vessels. ECF absorbed into a lymphatic vessel is called lymph, and it is returned to the circulatory system. Lymphatic vessels are more permeable than capillaries, having mini-valves on their outer edges. Mini-valves allow solids to enter the lymphatic vessels, including cellular debris, microorganisms, and cancer cells. The lymphatic vessels are connected to a number of lymph nodes, which clean up debris and mount an immune response against microorganisms and cancer cells. Knowing the anatomical connections of the lymphatic vessels helps locate areas of infection by the inflammation triggered in down-stream lymph nodes.
Lymph nodes
Lymph nodes are found throughout the body. A large cluster of lymph nodes can be found in the neck, called the cervical lymph nodes, in addition to other locations. Lymph nodes are composed primarily of reticular connective tissue, which provides support for resident clusters of white blood cells. Afferent lymphatic vessels bring lymph to the node, while efferent vessels drain lymph towards the circulatory system.
Tonsillar tissue
Tonsillar tissue is either a pseudostratified epithelium or a non-keratinized stratified squamous epithelium←, plus reticular connective tissue below. Tonsils are similar to lymph nodes, except there are no lymphatic vessels, and one end of the tonsil is un-encapsulated (the epithelial border). Clusters of white blood cells can be found in germinal centers, suspended within reticular connective tissue.
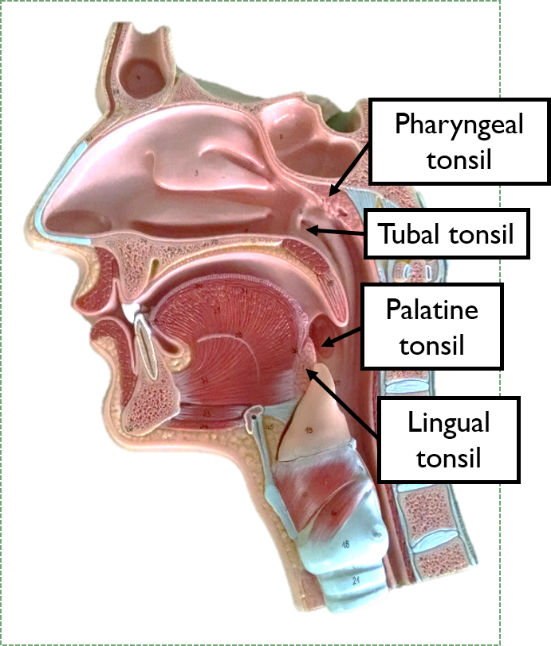
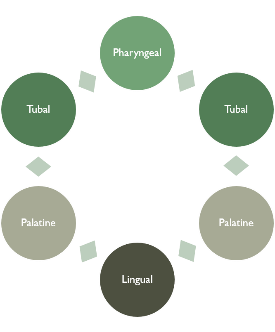
The tonsils
There are 4 major tonsils located the border of the oral cavity and pharynx: lingual, palatine, pharyngeal and tubal. These tonsils form a ring, called Waldeyer's ring, which serves to identify pathogens that are either ingested or inhaled, and begin an immune response before they reach deeper locations, such as the lungs or stomach. Because of their anatomy (no vessels), tonsils do not filter debris or microorganisms out of bodily fluids, they only identify pathogens. The un-encapsulated side faces the lumen of the pharynx, coming into contact with many foreign molecules.
Clinical applications of lymphatic system histology

"own work" by James Heilman MD, is licensed CC BY SA 3.0 / arrows addedLymphadenopathy of lymph nodes
In the absence of infection, lymph nodes are soft and moveable. However, if white blood cells detect a pathogen, they undergo cell division and release inflammatory molecules. This leads to lymph nodes becoming palpable, possibly visibly swollen, and likely sensitive to touch. The swelling of lymphatic tissue is called lymphadenopathy, and is a non-specific sign of immune system activation.

The mandibular incisors drain into sub-mental lymph nodes. The sub-mental lymph nodes and the rest of the teeth (other than maxillary 3rd molars) drain into sub-mandibular lymph nodes. The sub-mandibular lymph nodes then drain into superior deep cervical nodes. Swelling of some or all of these lymph nodes can indicate active periodontal disease.

"own work" by James Heilman MD, is licensed CC BY SA 3.0Lymphadenopathy of tonsillar tissue
Tonsillar tissue can become inflamed, and when it does it is usually called tonsillitis— when the increased number of white blood cells (living and dead) may be visible as white-ish patches within the inflamed tonsil(s). Tonsillitis is more common in children between pre-school and pre-teens because of the way the immune system develops immunocompetency and tolerance.
Para-nasal sinuses
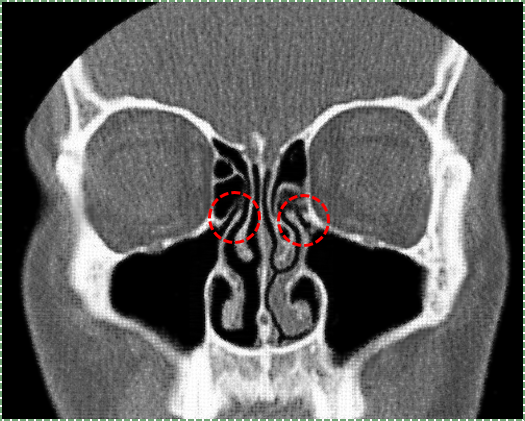
"conchae nasalis" by Simplicius, is licensed CC BY SA 3.0 / red circles addedBasic anatomy of the para-nasal sinuses
The para-nasal sinuses are spaces within the frontal, sphenoid, ethmoid and maxillary bones surrounding the nasal cavity. The maxillary, frontal and sphenoid sinus communicate with (connect to) the nasal cavity via small passageways. The para-nasal sinuses are lined with pseudostratified epithelium. This epithelium produces mucus which traps pathogens and debris. With the aid of cilia, these harmful agents are removed from the body. Within the nasal cavity are 3 bumps called nasal conchae, which divide the nasal cavity into three winding spaces called the nasal meatuses. (for those who are counting, there is a fourth space above the superior nasal conchae called the spheno-ethmoid recess, it is not a meatus because it does not form a pathway from the nasal vestibule to the nasopharynx).
Clinical applications of para-nasal sinus histology
"own work" by James Heilman MD, is licensed CC BY SA 3.0Inflammation within the para-nasal sinuses
When para-nasal sinuses become inflamed (known as sinusitis), the small ducts leading to the nasal sinuses may become obstructed. The increase in fluid that accompanies inflammation has nowhere to drain, leading to pressure within the sinuses. Furthermore, one response of goblet cells to inflammatory signals is to produce more mucous proteins, which again have nowhere to drain.
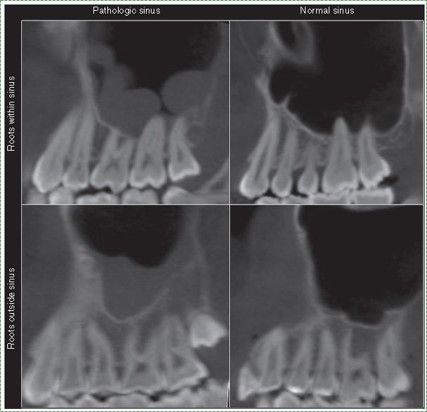
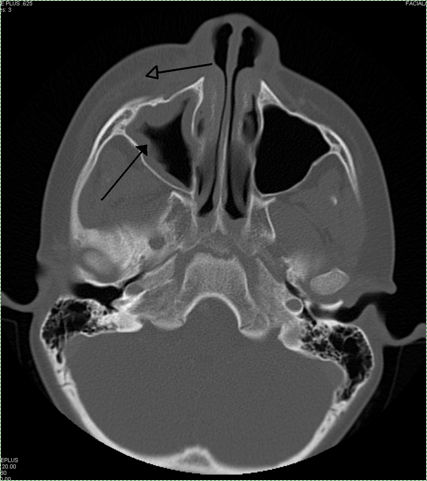
"Figure" by Gina Roque-Torres, is licensed CC BY 4.0The posterior maxillary teeth lie close to, or sometimes partly within the maxillary sinuses. Therefore, if inflammation occurs within these sinuses, it can cause discomfort to the significantly more-sensitive teeth. Furthermore, sinus infections may spread to the posterior maxillary teeth.
< Chapter 4 * navigation * Chapter 6 >
Chapter review questions
Secreting to a surface of the body, either the outer surface (skin) or inner surface (lumen of a hollow organ).
An epithelium composed of one layer of square cells
A small sac-like cavity in a gland, surrounded by secretory cells.
Epithelia that have one layer of tall cells
Connective tissue casing or outer border of an organ.
The main structural protein in the ECM of connective tissues
Rod-like mineralized connective tissue structures found in spongy-bone.
A soft connective tissue composed of reticular fibers, ground substance, plus fibroblasts and blood cells.
Sites within lymphoid organs where mature B cells proliferate and differentiate.
Watery liquid secreted into the mouth, providing lubrication for chewing and swallowing, and protection for the teeth.
The mucous membrane lining the inside of the mouth. It is a stratified squamous epithelium, named the oral epithelium, and an underlying areolar connective tissue named the lamina propria.
The process of converting DNA into an mRNA copy
The process of turning the sequence of a mRNA into a sequence of amino acids during protein synthesis
An adjective used to describe a gelatinous, slimy substance such as loose ground substance or mucus.
rough Endoplasmic Reticulum, an organelle where membrane and secreted proteins are translated by bound ribosomes on the surface of the rER.
A membrane-bound organelle that modifies proteins from the rER and packages them up into vesicles, to be sent to lysosomes, the plasma membrane, or secreted from the cell.
A protein that has had sugar residues attached to it in the Golgi apparatus and is often secreted.
the gelatinous material within a living cell, excluding organelles.
Hollow center or cavity inside a structure.
A protein film that forms on the surface enamel by binding of glycoproteins from saliva that prevents continuous deposition of salivary calcium phosphate.
Inflammation of gingival tissue
Damage to a tooth that can happen when decay-causing bacteria make acids that de-mineralize tooth tissues.
Glandular acini that produce watery secretions.
Hematoxylin and Eosin stain, typically turns proteins pink and DNA purple.
Glandular acini that secrete more gelatinous (or mucous) secretions.
Glandular acini that make a mixture of watery and gelatinous secretions.
Epithelial cells found in glands, containing smooth muscle actin allowing them to contract and expel secretions of exocrine glands.
A dynamic network of interlinking cytoplasmic proteins (mainly actin filaments, intermediate filaments and microtubules), involved in maintaining cell shape, polarity and migration.
Undifferentiated or partially differentiated cells that can differentiate into various cell types, and proliferate to produce more of the same stem cell.
deoxyribonucleic acid is the hereditary material in humans and almost all other organisms.
The developmental history of a differentiated cell traced back to the embryonic cell from which it arises.
When one cell begins to look different from another. This process involves limiting cell fate by altering gene transcription to become more specialized.
he most exterior of the three primary germ layers formed in the gastrula, it gives rise to the epithelial tissue covering the body and the CNS.
Multipotent cells of a connective tissue that can differentiate into a variety of cell types, including osteoblasts, fibroblasts, chondrocytes, myoblasts, blood cells and adipocytes.
A more differentiated form of a myo-satellite cell that can differentiate into a muscle cell (myofibril)
Two salivary glands that sit in front of the ears on each side of the face
Paired salivary glands on the floor of the oral cavity, underneath the tongue, bordered laterally by the mandible and medially by genioglossus muscle of the tongue.
Major salivary glands located beneath the floor of the mouth, superior to the digastric muscles.
Small salivary glands located throughout the oral cavity that generally get no name.
minor salivary glands associated with circumvallate papillae.
A highly contagious viral disease caused by the mumps virus, causing swelling of the parotid salivary gland(s).
Decreased saliva production.
The symptom of having a dry mouth due to reduced saliva production.
A signaling molecule capable of stimulating cell proliferation, wound healing, and cellular differentiation.
Calculus produced from saliva.
A mucous cyst
A cyst that forms in the mouth under the tongue.
Radiographic examination of the salivary glands, involving the injection of a contrast medium into the salivary duct of a single gland.
Extra-Cellular Fluid is the fluid surrounding cells, but not within blood or lymphatic vessels.
A type of connective tissue composed of cells (white blood cells) and ECM (lymph).
Similar to venous valves, mini-valves are on the walls of lymphatic vessels, allowing them to absorb larger materials than blood vessels.
A small bean-shaped structure that is part of the body's immune system.
300 (of 800 total) lymph nodes found in the neck.
An epithelium that has more than one layer of cells, but the layers are not organized into distinct rows.
A stratified squamous epithelium that does not contain the protein keratin, making it softer and moister than the skin.
Epithelia that have more than one layer of cells, with the cells at the apical surface having a flat shape.
Four tonsils (pharyngeal, tubal, palatine and lingual tonsils) as well as small collections of lymphatic tissue disbursed throughout the mucosal lining of the pharynx.
Palpable enlargement of lymph nodes.
Lymph nodes in the mental region whose afferent vessels drain central portions of the lower lip, floor of the mouth and apex of the tongue, and whose efferent vessels drain partly into sub-mandibular lymph nodes and partly into deep cervical lymph nodes.
Three to six lymph nodes beneath the body of the mandible in the sub-mandibular triangle, or the superficial surface of the sub-mandibular gland, whose afferent vessels drain the medial canthus, cheek, side of the nose, upper lip, lateral part of the lower lip, gums, and the anterior part of the margin of the tongue, and whose efferent vessels drain ino the superior deep cervical lymph nodes.
Lymph nodes under the sternocleidomastoid muscle.
Inflammation of the tonsils
Spaces within the frontal, sphenoid, ethmoid and maxillary bones surrounding the nasal cavity.
A thin gelatinous secretion composed of primarily of glycoproteins and water.
Inflammation of the sinuses.
Unicellular glands, or single epithelial cells, that secrete mucus.

