Health Equity
Elizabeth B. Pearce; Amy Huskey; Jessica N. Hampton; and Hannah Morelos
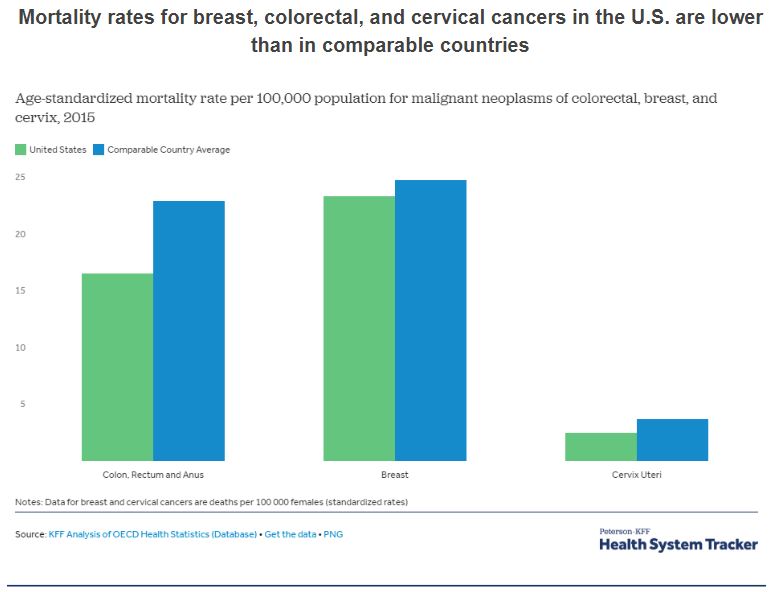
Health in the United States is a complex topic. One the one hand, as one of the wealthiest nations, the United States fares well in some health comparisons with the rest of the world. For example, most postoperative complications are less common in the U.S. than in comparable countries. And, as this chart shows, mortality rates for several cancers are lower.
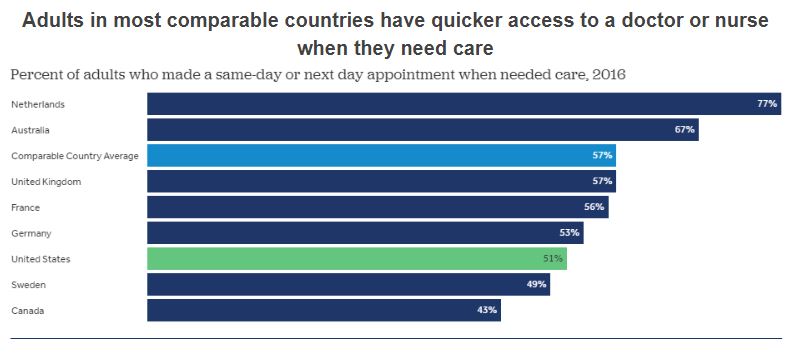
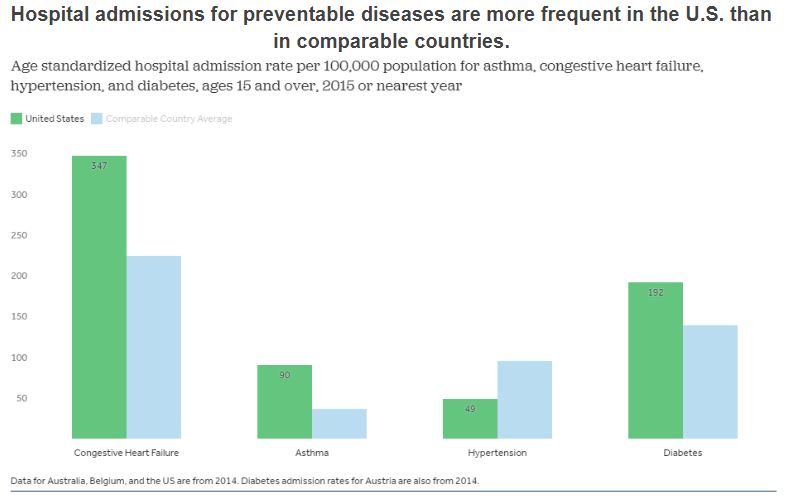
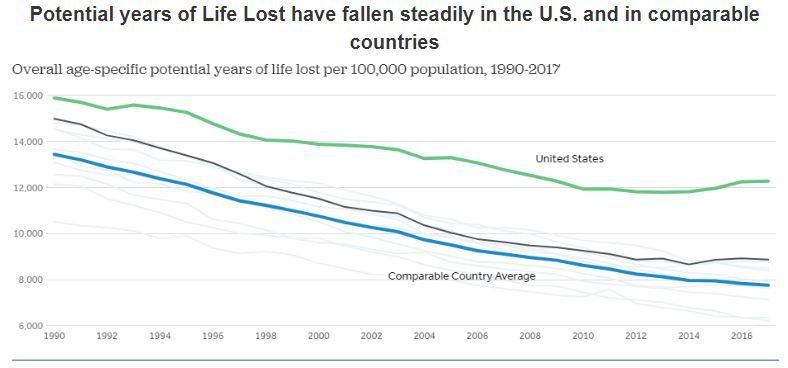
The overall comparative picture is more grim. The United States spends a great deal more public, private, and out-of pocket funds per capita on health care[1] but also lags behind almost every industrialized country in terms of providing basic health and health care to all of its citizens.
But these charts do not tell the entire story. The overall averages of health only compare the rates in the U.S. to the rates in other countries. Within the United States, groups are affected disproportionately in terms of access to health and health outcomes. These disparities are described next.
Social Determinants of Health and Disparities
Family and individual health is affected by the environments in which people live, work, learn, and play. While the focus here is health, these social determinants of health also affect a wide range of quality of life factors. Social engagement, access to resources, safety and security are all impacted by the settings where families spend their time. Simply put, place matters when it comes to health. To read more about the Social Determinants of Health model, consult https://health.gov/healthypeople.
Health disparities are linked to the social determinants of health. They are preventable differences in the burden of disease, injury, violence, or opportunities to achieve optimal health that are experienced by socially disadvantaged populations.[2] Populations can be defined by factors such as race or ethnicity, gender, education or income, disability, geographic location (e.g., rural or urban), or sexual orientation. Health disparities are inequitable and are directly related to the historical and current unequal distribution of social, political, economic, and environmental resources.
Health disparities result from multiple factors, including
- Poverty
- Environmental threats
- Inadequate access to health care
- Individual and behavioral factors
- Educational inequalities
Health disparities are also related to inequities in education. Dropping out of school is associated with multiple social and health problems.[3][4] Overall, individuals with less education are more likely to experience a number of health risks, such as obesity, substance abuse, and intentional and unintentional injury, compared with individuals with more education.[5] Higher levels of education are associated with a longer life and an increased likelihood of obtaining or understanding basic health information and services needed to make appropriate health decisions.[6][7][8]
At the same time, good health is associated with academic success. Higher levels of protective health behaviors and lower levels of health risk behaviors have been associated with higher academic grades among high school students.[9] Health risks such as teenage pregnancy, poor dietary choices, inadequate physical activity, physical and emotional abuse, substance abuse, and gang involvement have a significant impact on how well students perform in school.[10][11][12][13][14]
Health by Race and Ethnicity
When looking at the social epidemiology of the United States, it is hard to miss the disparities among races. The discrepancy between Black and White Americans shows the gap clearly; in 2008, the average life expectancy for White males was approximately five years longer than for Black males: 75.9 compared to 70.9. An even stronger disparity was found in 2007: the infant mortality, which is the number of deaths in a given time or place, rate for Blacks was nearly twice that of Whites at 13.2 compared to 5.6 per 1,000 live births[15]. According to a report from the Henry J. Kaiser Foundation,[16] African Americans also have higher incidence of several other diseases and causes of mortality, from cancer to heart disease to diabetes. In a similar vein, it is important to note that ethnic minorities, including Mexican Americans and Native Americans, also have higher rates of these diseases and causes of mortality than Whites.
Lisa Berkman[17] notes that this gap started to narrow during the Civil Rights movement in the 1960s, but it began widening again in the early 1980s. What accounts for these perpetual disparities in health among different ethnic groups? Much of the answer lies in the level of healthcare that these groups receive. Even after adjusting for insurance differences, racial and ethnic minority groups receive poorer quality of care and less access to care than dominant groups.[18] Racial inequalities in care include:
- Black Americans, Native Americans, and Alaskan Natives received inferior care than White Americans for about 40 percent of measures.
- Asian ethnicities received inferior care for about 20 percent of measures.
- Among Whites, Hispanic Whites received 60 percent inferior care of measures compared to non-Hispanic Whites.
- When considering access to care, the figures were comparable.
Health by Socioeconomic Status (SES)
Discussions of health by race and ethnicity often overlap with discussions of health by socioeconomic status, since the two concepts are intertwined in the United States. As the Agency for Health Research and Quality (2010) notes, “racial and ethnic minorities are more likely than non-Hispanic Whites to be poor or near poor,”[19] so many of the data pertaining to subordinate groups is also likely to be pertinent to low socioeconomic groups. Marilyn Winkleby and her research associates[20] state that “one of the strongest and most consistent predictors of a person’s morbidity and mortality experience is that person’s socioeconomic status (SES). This finding persists across all diseases with few exceptions, continues throughout the entire lifespan, and extends across numerous risk factors for disease.” Morbidity is the incidence of disease.
It is important to remember that economics are only part of the SES picture; research suggests that education also plays an important role. Phelan and Link[21] note that many behavior-influenced diseases like lung cancer (from smoking), coronary artery disease (from poor eating and exercise habits), and AIDS initially were widespread across SES groups.
However, once information linking habits to disease was disseminated, these diseases decreased in high SES groups and increased in low SES groups. This illustrates the important role of education initiatives regarding a given disease, as well as possible inequalities in how those initiatives effectively reach different SES groups.
Health by Gender
Women are affected adversely both by unequal access to and institutionalized sexism in the healthcare industry. According to a recent report from the Kaiser Family Foundation, women experienced a decline in their ability to see needed specialists between 2001 and 2008. In 2008, one quarter of females questioned the quality of her healthcare[22]. In this report, we also see the explanatory value of understanding intersectionality and intersection theory. Feminist sociologist Patricia Hill Collins developed the intersection theory, which suggests we cannot separate the effects of race, class, gender, sexual orientation, and other attributes. Further examination of the lack of confidence in the healthcare system by women, as identified in the Kaiser study, found, for example, women categorized as low income were more likely (32 percent compared to 23 percent) to express concerns about healthcare quality, illustrating the multiple layers of disadvantage caused by race and sex.
We can see an example of institutionalized sexism in the way that women are more likely than men to be diagnosed with certain kinds of mental disorders. Psychologist Dana Becker[23] notes that 75 percent of all diagnoses of Borderline Personality Disorder (BPD) are for women, according to the Diagnostic Statistical Manual of Mental Disorders. This diagnosis is characterized by instability of identity, of mood, and of behavior, and Becker argues that it has been used as a catch-all diagnosis for too many women. She further decries the pejorative connotation of the diagnosis, saying that it predisposes many people, both within and outside of the profession of psychotherapy, against women who have been so diagnosed.
Many critics also point to the medicalization of women’s issues as an example of institutionalized sexism. Medicalization refers to the process by which previously normal aspects of life are redefined as deviant and needing medical attention to remedy. Historically and contemporaneously, many aspects of women’s lives have been medicalized, including menstruation, premenstrual syndrome, pregnancy, childbirth, and menopause. The medicalization of pregnancy and childbirth has been particularly contentious in recent decades, with many women opting against the medical process and choosing a more natural childbirth. Fox and Worts[24] find that all women experience pain and anxiety during the birth process, but that social support relieves both as effectively as medical support. In other words, medical interventions are no more effective than social ones at helping with the difficulties of pain and childbirth. Fox and Worts further found that women with supportive partners ended up with less medical intervention and fewer cases of postpartum depression. Of course, access to quality birth care outside the standard medical models may not be readily available to women of all social classes.
The Lancet, an international peer-reviewed general medical journal, is published weekly and available to read online without cost. In 2017, they published a comprehensive series about inequality and health care in the United States. The Table of Contents for the series is linked here; although it is free, you will need to log in to read the series of articles.
Interrelationship of Mental and Physical Health
Mental and physical health have been socially constructed in the Western world to be viewed as separate, with mental disorders being stigmatized. Often mental illnesses such as depression or anxiety have been seen as something that a person should and could “get over” as opposed to a physical ailment such as a sprained ankle or strep throat that merits medical attention and assistance. Even physical illnesses such as fibromyalgia or chronic fatigue syndrome, which are experienced by many more women than men, can be seen as “in the patient’s head,” leading to the potential miss of physical illnesses that need medical intervention. This leaves the patient with not only the physical symptoms, but also a potential lack of understanding amongst peers, family members, medical professionals, and co-workers.
Eastern and Native cultures have long seen the connection between the mind and body and indeed, this connection is better understood in the United States and among other Western countries where dualism (the separating of the mind/spirit from the body) prevails. Cancer, heart and respiratory disease death rates are all higher in people with mental illness. In addition, it is better understood how physical lifestyle choices such as exercise, diet, and drug use affect mental health and vice versa.[25] To read more about the relationship between physical and mental health, check out this brief article from PsychCentral here.
Stigma
An example of the relationship between mental health and stigma would be a person struggling with depression that also causes a physical symptom of weight gain or weight loss due to a lack of appetite or excessive hunger. Obesity and excessive thinness are both stigmatized in our culture, while the underlying mental or physical health condition may be ignored. Mental health disorders are treated and looked at differently than health struggles on a more physical level. Although we have seen a shift in media about mental illness from known celebrities coming forward, such as Demi Lovato, Chrissy Teigan, Steve Young, and Dan Reynolds, there is still a social stigma against mental health. Oftentimes, when someone is diagnosed with a physical illness such as cancer or heart disease, we see communities and families coming together. Unfortunately, we rarely see mental illness struggles come to the surface without holding a place of shame or guilt; individuals, families and communities are often more reluctant to talk about and come together in the same way.

When we speak about stigma, we speak of two different types: the first stigma is social stigma, meaning the prejudiced attitudes others have around mental illness and the treatment of mental illness. The second one is self-perceived stigma, which is an internalized stigma that the individual who suffers from the mental illness has. Not only may the stigma around mental illness create painful emotions and a sense of invalidation for the individual, it can result in a reluctance to seek treatment, social rejection, avoidance, isolation, and direct harm to psychological well-being. The social and self-perceived stigma attached to mental illness can be reinforced by common cultural misconceptions, social stereotypes, popular media representations, political leaders, and even some medical professionals and health care institutions.
Health Insurance Coverage and Legislation
Like all other health care in the United States, access to mental health care is highly dependent on access to medical insurance. But because the need for mental health support is not validated as fully as is the need for physical health support, insurance companies and government programs have frequently excluded or limited mental health coverage. This is an example of institutionalized or structural stigma.
This practice has been changed through two major acts of legislation; the Mental Health Parity and Addiction Equity Act (MHPAEA) passed in 2008 and The Patient Protection and Affordable Care Act, commonly referred to as the Affordable Care Act (ACA) and also known as Obamacare, passed by the 111th Congress and signed into law by President Barack Obama in 2010.
In 2008, federal lawmakers passed MHPAEA, which created an equity requirement for insurance providers who covered mental health services; those services must be equivalent to the physical health coverage provided. It did not, however, require providers to provide mental health care coverage. So benefits, expenses, and limits requirements were allowed to vary from state to state along with whatever insurance plan individuals could access. It was still the case that insurance holders did not have access to mental health treatment. In 2013, 61% of insured people had access to mental health services and 54% of the insured had access to addiction treatment.[26]
The passage of the ACA reduced the inequities in access to mental health and addiction treatment in two fundamental ways. First, it eliminated health insurance companies’ ability to deny coverage based on “pre-existing conditions.” That gave consumers diagnosed with any mental or physical illness greater choice and more financial leverage when selecting an insurance company. In addition, it required insurance providers to include ten essential benefits including “services for those suffering from mental health disorders and problems with substance abuse.” To read the list of all ten benefits, look here.
While these improvements in the equitability of mental health and addiction access are notable, they apply only to families who have access to certain kinds of health insurance, and not universally to all families in the United States. Structural stigma pollinates and overlaps with systemic racism, sexism, and classism.
In Focus: Sleep, Discrimination, and Intersectionality
Let’s focus on how these various disparities overlap with everyday behavior. A biological need that is fundamental to human health is sleep, yet the medical community still has much to understand and learn about its exact mechanisms. Sleep is a vital part of our daily routine, and we spend about one-third of our time doing it. Quality sleep, and getting enough of it at the right times, is as essential to survival as food and water. In rats, death results from no sleep at 32 days.[27] Research has not observed human death as a result of prolonged sleep deprivation, but paranoia and hallucinations can begin happening in as little as 24 hours without sleep.[28]
Without sleep you can’t form or maintain the pathways in your brain that let you learn and create new memories, and it’s harder to concentrate and respond quickly. Sleep is important to a number of brain functions, including how nerve cells communicate with each other. In fact, our brains and bodies stay remarkably active while we sleep. Recent findings suggest that sleep plays a housekeeping role that removes toxins in our brains that build we are awake.
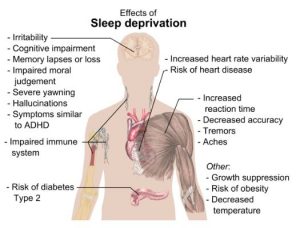
Sleep affects almost every type of tissue and system in the body, from the brain, heart, and lungs to metabolism, immune function, mood, and disease resistance. Research shows that a chronic lack of sleep, or getting poor quality sleep, increases the risk of disorders including high blood pressure, cardiovascular disease, diabetes, depression, and obesity. All of these conditions would likely have a noticeable effect on multiple dimensions of family life and how it impacts the well being of a family as a whole.
For some surprising and specific health effects of sleep view this TED Talk:
In 2010, a study was published that examined whether there were disparities in sleep quality based on poverty and race/ethnicity. They found that a “sleep disparity” did exist in the study population, and poor sleep quality was strongly associated with poverty and race. Factors such as employment, education, and health status, amongst others, significantly mediated this effect in participants experiencing poverty. The literature linking sleep and health continues to grow. This study illustrated how poor health is associated with an almost 4-fold increased likelihood of poor sleep. It is important to note that the relationship between health and sleep quality is likely bidirectional and/or parallel: sleep can influence health and vice versa.[29]
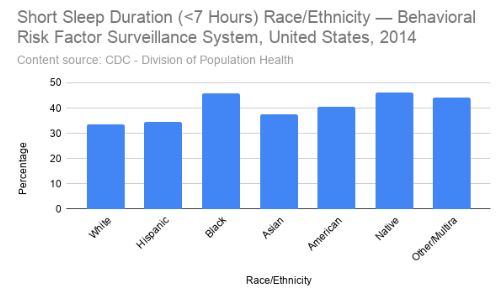
Discrimination, and especially intersectional discrimination, appear to influence sleep, mental, and physical health. The relationship between discrimination and poorer mental and physical health has been established amongst populations such as women, racial and ethnic minorities, and members of LGBTQ+ groups. For instance, discrimination can harm wellbeing, increase distress and mental illness symptoms, elevate risk for a wide variety of physical illnesses and conditions, and undermine general indicators of health.[30][31] Consider also the ways that poor and marginalized groups inhabit less desirable neighborhoods. The overlap of all social determinants of health and feeling safe and secure in particular are likely to impact sleep. Recently, lack of sleep and less functionality during the daytime have been identified as integral aspects of the cycle of discrimination, stress, and overall mental and physical health.[32]
Licenses and Attributions
Open Content, Shared Previously
“Disparities” is adapted from “Health Disparities” by the Centers for Disease Control and Prevention. Public domain. [Adaptation: ?]
“Health by Race and Ethnicity,” “Healthy by Socioeconomic Status,” and “Healthy by Gender” are adapted from “Health in the United States” in Introduction to Sociology 2e. License: CC BY 4.0. [Adaptation: ?]
“In Focus: Sleep, Discrimination and Intersectionality” is adapted from “Brain Basics: Understanding Sleep” by the National Institute of Neurological Disorders and Stroke / National Institute of Health. Public domain. Adaptations: Changed just a few words and changed some hyphens to commas.
Figure 3.3. “Mortality rates for breast and colorectal cancer in the U.S. are lower than in comparable countries” by Peterson-KFF. License: CC BY-NC-ND 3.0.
Figure 3.4. “Percent of adults who made a same-day or next day appointment when needed care, 2016” by Peterson-KFF. License: CC BY-NC-ND 3.0.
Figure 3.5. “Age-sex standardized hospital admission rate per 100,000 population for asthma, congestive heart failure, hypertension, and diabetes, ages 15 and over, 2016 or nearest year” by Peterson-KFF. License: CC BY-NC-ND 3.0.
Figure 3.6. “Potential Years of Life Lost have fallen steadily in the U.S. and in comparable OECD countries” by Peterson-KFF. License: CC BY-NC-ND 3.0.
Figure 3.7. “Right on” by LizSpikol. Licensed under CC BY-NC-ND 2.0.
Figure 3.8. “Main health effects of sleep deprivation” by Mikael Häggström. CC0.
Figure 3.9. “Short sleep duration (<7 hours) race/ethnicity” by CDC. Public domain.
All Rights Reserved Content
“Sleep is your superpower” (c) TED Talks. License Terms: Standard YouTube license.
- Tikkanen, R. & Abrams, M.K. (2020, January 30). U.S. health care from a global perspective, 2019: Higher spending, worse outcomes? The Commonwealth Fund. https://www.commonwealthfund.org/publications/issue-briefs/2020/jan/us-health-care-global-perspective-2019 ↵
- CDC. (2008). Community Health and Program Services (CHAPS): Health disparities among racial/ethnic populations. Atlanta: U.S. Department of Health and Human Services. ↵
- McCarty, C. A., Mason, W. A., Kosterman, R., Hawkins, J. D., Lengua, L. J., & McCauley, E. (2008). Adolescent school failure predicts later depression among girls. Journal of Adolescent Health, 43(2), 180–187. https://doi.org/10.1016/j.jadohealth.2008.01.023 ↵
- Ellickson, P., Saner, H., & McGuigan, K. A. (1997). Profiles of violent youth: Substance use and other concurrent problems. American Journal of Public Health, 87(6), 985–991. https://doi.org/10.2105/AJPH.87.6.985 ↵
- U.S. Department of Health and Human Services. (2000). Healthy People 2010 objectives: Educational and community based programs. ↵
- Liao, Y., McGee, D. L., Kaufman, J. S., Cao, G., & Cooper, R. S. (1999). Socioeconomic status and morbidity in the last years of life. American Journal of Public Health, 89(4), 569–572. https://doi.org/10.2105/AJPH.89.4.569 ↵
- Jemal, A., Thun, M. J., Ward, E. E., Henley, S. J., Cokkinides, V. E., & Murray, T. E. (2008). Mortality from leading causes by education and race in the united states, 2001. American Journal of Preventive Medicine, 34(1), 1-8.e7. https://doi.org/10.1016/j.amepre.2007.09.017 ↵
- Breese, P. E., Burman, W. J., Goldberg, S., & Weis, S. E. (2007). Education level, primary language, and comprehension of the informed consent process. Journal of Empirical Research on Human Research Ethics, 2(4), 69–79. https://doi.org/10.1525/jer.2007.2.4.69 ↵
- Rasberry, C. N., Tiu, G. F., Kann, L., McManus, T., Michael, S. L., Merlo, C. L., Lee, S. M., Bohm, M. K., Annor, F., & Ethier, K. A. (2017). Health-related behaviors and academic achievement among high school students—United states, 2015. MMWR. Morbidity and Mortality Weekly Report, 66(35), 921–927. https://doi.org/10.15585/mmwr.mm6635a1 ↵
- Choi, Y. (2007). Academic achievement and problem behaviors among Asian Pacific Islander American adolescents. Journal of Youth and Adolescence, 36(4), 403–415. https://doi.org/10.1007/s10964-006-9152-4 ↵
- Shore, S. M., Sachs, M. L., Lidicker, J. R., Brett, S. N., Wright, A. R., & Libonati, J. R. (2008). Decreased scholastic achievement in overweight middle school students. Obesity, 16(7), 1535–1538. https://doi.org/10.1038/oby.2008.254 ↵
- Valois, R. F., MacDonald, J. M., Bretous, L., Fischer, M. A., & Drane, J. W. (2002). Risk factors and behaviors associated with adolescent violence and aggression. American Journal of Health Behavior, 26(6), 454–464. https://doi.org/10.5993/AJHB.26.6.6 ↵
- Chomitz, V. R., Slining, M. M., McGowan, R. J., Mitchell, S. E., Dawson, G. F., & Hacker, K. A. (2009). Is there a relationship between physical fitness and academic achievement? Positive results from public school children in the northeastern united states. Journal of School Health, 79(1), 30–37. https://doi.org/10.1111/j.1746-1561.2008.00371.x ↵
- Field, T., Diego, M., & Sanders, C. E. (2001). Exercise is positively related to adolescent's relationships and academics. Adolescence, 36(141), 105. ↵
- U.S. Census Bureau. (2011). Statistical Abstract of the United States: 2012. 131st ed. Washington, DC. http://www.census.gov/compendia/statab. ↵
- James, C. et al. (2007). Key facts: Race, ethnicity & medical care. The Henry J. Kaiser Family Foundation. http://www.kff.org/minorityhealth/upload/6069-02.pdf. ↵
- Berkman, L. F. (2009). Social epidemiology: Social determinants of health in the united states: are we losing ground? Annual Review of Public Health, 30(1), 27–41. https://doi.org/10.1146/annurev.publhealth.031308.100310 ↵
- Agency for Healthcare Research and Quality. (2010). The 2010 National Healthcare Disparities Report. https://archive.ahrq.gov/research/findings/nhqrdr/nhdr10/index.html ↵
- footnote]Agency for Healthcare Research and Quality. (2010). The 2010 National Healthcare Disparities Report. https://archive.ahrq.gov/research/findings/nhqrdr/nhdr10/index.html ↵
- Winkleby, M. A., Jatulis, D. E., Frank, E., & Fortmann, S. P. (1992). Socioeconomic status and health: How education, income, and occupation contribute to risk factors for cardiovascular disease. American Journal of Public Health, 82(6), 816–820. https://doi.org/10.2105/AJPH.82.6.816 ↵
- Phelan, Jo C., & Link, B. G. (2003). When income affects outcome: Socioeconomic status and health. Research in Profile, 6. ↵
- Ranji, U., & Salganico, A. (2011). “Women's health care chartbook: Key findings from the Kaiser Women's Health Survey.” The Henry J. Kaiser Family Foundation. https://www.kff.org/womens-health-policy/report/womens-health-care-chartbook-key-findings-from/ ↵
- Becker, Dana. n.d. Borderline Personality Disorder: The disparagement of women through diagnosis.” Retrieved December 13, 2011 from http://www.awpsych.org/index.php?option=com_content&view=article&id=109&catid=74&Itemid=126. ↵
- Fox, B., & Worts, D. (1999). Revisiting the critique of medicalized childbirth: A contribution to the sociology of birth. Gender & Society, 13(3), 326–346. https://doi.org/10.1177/089124399013003004 ↵
- Mental Health Foundation. (2020). Physical health and mental health. Retrieved July 3, 2020, from https://www.mentalhealth.org.uk/a-to-z/p/physical-health-and-mental-health ↵
- Health Pocket. (2013, March 7). Few existing health plans meet new ACA essential health benefit standards. https://www.healthpocket.com/healthcare-research/infostat/few-existing-health-plans-meet-new-aca-essential-health-benefit-standards ↵
- Palmer, B. (2009, May 11). Can you die from lack of sleep? Slate. https://slate.com/news-and-politics/2009/05/can-you-die-from-lack-of-sleep.html ↵
- Waters, F., Chiu, V., Atkinson, A., & Blom, J. D. (2018). Severe sleep deprivation causes hallucinations and a gradual progression toward psychosis with increasing time awake. Frontiers in Psychiatry, 9, 303. https://doi.org/10.3389/fpsyt.2018.003 ↵
- Patel, N. P., Grandner, M. A., Xie, D., Branas, C. C., & Gooneratne, N. (2010). “Sleep disparity” in the population: Poor sleep quality is strongly associated with poverty and ethnicity. BMC Public Health, 10(1), 475. https://doi.org/10.1186/1471-2458-10-475 ↵
- Brown, T. T., Partanen, J., Chuong, L., Villaverde, V., Chantal Griffin, A., & Mendelson, A. (2018). Discrimination hurts: The effect of discrimination on the development of chronic pain. Social Science & Medicine, 204, 1–8. https://doi.org/10.1016/j.socscimed.2018.03.015 ↵
- Schmitt, M. T., Branscombe, N. R., Postmes, T., & Garcia, A. (2014). The consequences of perceived discrimination for psychological well-being: A meta-analytic review. Psychological Bulletin, 140(4), 921–948. https://doi.org/10.1037/a0035754 ↵
- Hisler, G. C., & Brenner, R. E. (2019). Does sleep partially mediate the effect of everyday discrimination on future mental and physical health? Social Science & Medicine, 221, 115–123. https://doi.org/10.1016/j.socscimed.2018.12.002 ↵
The settings and conditions in which individuals and families spend most of their time, which affect their health and quality of life.
Lack of fair treatment, opportunity, or conditions.
The combination of one’s social and economic status, specifically related to income, education, and career or job status.
An approach originally advanced by women of color that finds it critical to look at how identities and characteristics (such as ethnicity, race, gender, etc.) overlap and influence each other to create complex hierarchies of power and oppression.

