7.2 Health, Wellness, Sickness, and Disease
Elizabeth B. Pearce and Amy Huskey
“It is health that is real wealth and not pieces of gold and silver.”
— Mahatma Gandhi
Health is the “state of complete physical, mental and social well-being and not merely the absence of disease or infirmity,” as defined by the World Health Organization (WHO) (2005) in its Constitution. The organization goes on to state that families and communities are able to thrive when individuals are able to maintain health. Our employment, finances, mental and emotional functioning, and spiritual lives all interact with our overall health.
While the status of health is very real, it is also important to examine the aspects of health and illness that are socially constructed. As members of society, we share assumptions about reality that define both health and illness. Illness has a biological component, yet it also embodies an independent element that is experienced by the person and observed by those outside of the illness. Societies construct the idea of “health” differently from place to place, and over time. For example, many societies consider health and health care to be a human right that all human beings are entitled to, but this is not universally true (Figure 7.1). What is your viewpoint?
The social construction of the idea of family, as discussed in Chapter 1, plays a special role in the health of families in the United States. In all other industrialized countries, health care is considered a human right, and all individuals can access comparable care regardless of family status. But in the U.S., health care insurance is accessed through a variety of systems, all of which have age, income, employment status, and family relationships as criteria. How do definitions of “family” impact the access of any individual to health care?

Figure 7.1. Activists around the world continue to strive for universal access to health care.
Society informs the definitions for when an illness can be considered a disability, how eligibility for insurance and medical coverage are determined, what illnesses are perceived as legitimate, when the reality of an illness is questioned, and what illnesses are stigmatized (Griffiths & Keirns, 2015). These social constructs can, in themselves, contribute to differentiation in individual health as well as stereotypes, prejudice, and discrimination. Stigma, the social process whereby individuals that are taken to be different in some way are rejected by the greater society in which they live based on that difference, operates in the world of health, ability, and illness. Sociologist Erving Goffman said, “Stigma is a process by which the reaction of others spoils normal identity.” A disease or illness that is stigmatized is one in which there is some societal disapproval or questioning of the integrity of people who have the disease, which can also include medical professionals and the person with the disease stigmatizing themselves (Figure 7.2).
Figure 7. 2. Stigma – Social and self | Individuals and Society | MCAT | Khan Academy [YouTube Video]. The Khan Academy Medicine channel describes the interrelationship among stigma, self, and society in this 7-minute video.
There are many socially stigmatized diseases which can include mental disorders, HIV/AIDS and other sexually transmitted diseases, substance abuse disorders, skin conditions, and diseases that are less understood by the medical community, such as auto-immune disorders and chronic fatigue syndrome. Individuals may be less likely to seek treatment when experiencing symptoms of a stigmatized condition. In the United States, where health insurance creates another layer of bureaucracy, less understood illnesses and treatments may not be covered by some insurance.
Even if a person with a stigmatized disease accesses health care, they may have fewer social supports and greater chances of isolation and discrimination in the health care setting and beyond. Management of a disability because of the deterioration of health due to a stigmatized illness can prove to be a tremendous hardship (Sartorius, 2007). It is important to consider how marginalized groups experience health inequities, including those experienced due to the stigma and prejudices linked with the societal perception of specific illnesses.
One’s status in society, or structural power, can complicate the experience of social stigma related to medical conditions. For example, cisgender men hold more power in the United States than women or people outside the gender binary. What role does that play in the diagnosis of real health concerns and the social construction of those concerns?
We know that overwhelmingly men are the subjects of the majority of medical studies and research. That affects what is thought of as “typical” or “normal.” Women have more often been told that their symptoms are “all in your head” or related to “female troubles.” While this is less common than in the past, it likely continues to play a part in the misdiagnosis of serious illness in women and people with nonbinary gender identities. We also know that women experience diseases such as myalgic encephalomyelitis/chronic fatigue syndrome and fibromyalgia in much higher numbers than do men. The medical community describes these syndromes in overly broad terms that make diagnosis difficult. We must ask ourselves, how do these multiple complex factors serve to continue to reinforce the existing power dynamic in the United States? What systemic changes in healthcare would reduce this inequity?
In this chapter, we will examine the overall health of families in the United States, with attention to comparisons among families’ experiences with health, illness, injury, and diseases as well as comparisons with other countries. We will describe the daily life factors and resources that affect health, including the effects of stigma, prejudice and discrimination. We will look closely at how families access health care services, including the health care insurance system. We will discuss the question of health care as a human right.
7.2.1 Activity: Lung Cancer, Stigma, and Intersectionality
In a 2014 report, “Addressing the Stigma of Lung Cancer,” the American Lung Association (ALA) described how stigma can contribute to patients avoiding or delaying care when symptoms are experienced and how they may resist disclosing health information to providers. Patients could also experience fewer social supports, feel more distress related to the disease, experience additional conflicts in relationships, and receive lower quality of health care. The report then explained how the stigmas around lung cancer related to lung cancer being hard to detect early, being seen as a death sentence with little hope for survival, and being labeled “a smoker’s disease.” This could contribute to society’s feeling that people with lung cancer are to blame for their disease and ought to feel ashamed.
According to the ALA survey, the public lacked knowledge regarding the prevalence and mortality of lung cancer, as well as knowledge about the funding levels for research. Responders also lacked knowledge of factors, other than smoking, that contributed to the development of lung cancer, such as genetics and occupational or environmental exposures. Lack of knowledge could play an important role in perpetuating some of the negative associations with and assumptions related to lung cancer (Figure 7.3).
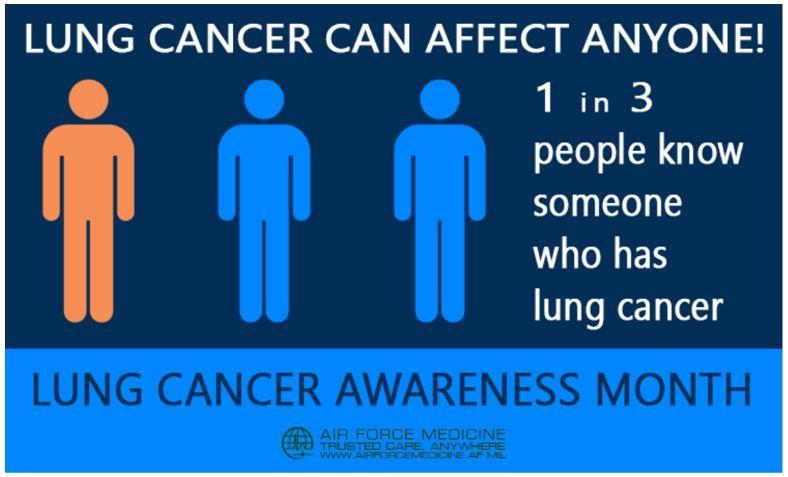
Figure 7.3. This graphic, created by the Air Force Medicine Facebook group, raises awareness about the commonality of lung cancer, which can help reduce stigma related to the disease.
Lung cancer stigma has real consequences. People with lung cancer may hide their condition and experience anxiety and depression. They may believe that healthcare providers are judgmental and biased towards them. Research, advocacy, and public policy are also dimensions in which stigma can have negative consequences for advancing progress toward the treatment of this disease. For instance, lung cancer kills far more people than any other cancer type and contributes to over 25 percent of all cancer deaths per year (American Cancer Society, 2020). Yet, a study of nonprofit research funding by cancer type determined that lung cancer ranked fourth in its level of funding and is underfunded in relation to its burden on society (Kamath et al., 2019). Not only are funding levels influenced by stigma, but celebrities, community leaders, and volunteers may be less likely to lend their name or volunteer their time due to negative associations with this disease (American Lung Association, 2014).
Discussion
- As you finish reading this section, notice if you blame or hold people more responsible knowing that they have lung cancer, than if they have another cancer such as breast or prostate cancer.
- What did you learn that was new or surprised you?
- What effect could the stigma itself have on people who are sick, and the healthcare that they receive?
- Is the stigmatization of lung cancer a social problem? Rather than perceiving lung cancer as a personal problem does the prevalence of the illness combined with the stigmatization affect the well-being of our society?
Understanding intersectionality and stigma provides a way of analyzing how intersectionality can be illustrated through the lens of the social construction of illness. The LGBTQ+ community, for instance, already faces challenges in finding health care providers who are culturally competent and have adequate knowledge in LGBTQ+ health (U.S. Dept. of Health and Human Services, n.d.). If you couple this with the stigma related to a lung cancer diagnosis, then you are compounding the obstacles that stand in the way of receiving quality health care. One could also examine how socioeconomic status may further complicate this scenario by realizing that people living in poverty are more likely to have no health insurance, therefore restricting access even more (U.S. Census Bureau, 2019). Even geographical location, like living in a rural area, or in the Southern portion of the United States, will reduce accessibility to healthcare (Warshaw, 2017). Every time an individual is grouped into a marginalized group, including illness status, it intensifies the effects of discrimination and resulting health disparities.
7.2.2 Licenses and Attributions for Health, Wellness, Sickness, and Disease
7.2.2.1 Open Content, Original
“Health, Wellness, Sickness, and Disease” by Elizabeth B. Pearce and Amy Huskey is licensed under CC BY 4.0.
7.2.2.2 Open Content, Shared Previously
Figure 7.1. “Chalking the Universal Declaration of Human Rights 2015″ by University of Essex. Licensed under CC BY-NC 2.0
“Activity: Lung Cancer, Stigma, and Intersectionality” is adapted by Elizabeth B. Pearce from “Health and Medicine” in Introduction to Sociology 2e.
_____________________Figure 7.2. “Lung Cancer Awareness” by Steve Thompson/ Air Force Medicine. Public domain.
Figure 7.3. “Stigma – Social and self | Individuals and Society | MCAT” by Khan Academy and AAMC. Licensed under CC BY-NC-SA 3.0.
7.2.3 References
World Health Organization. (2005, September 15). Constitution. Retrieved December 30, 2019, from https://www.who.int/about/who-we-are/constitution
OpenStax. (2015, April 24). Introduction to Sociology 2e. Retrieved March 8, 2020, from https://openstax.org/books/introduction-sociology-2e/pages/19-1-the-social-construction-of-health
Sartorius, N. (2007). Stigmatized illnesses and health care. Croatian Medical Journal, 48(3), 396–397.
American Cancer Society. (2020, January 8). Lung cancer statistics: How common is lung cancer. https://www.cancer.org/cancer/lung-cancer/about/key-statistics.htm
Kamath, S. D., Kircher, S. M., & Benson, A. B. (2019). Comparison of cancer burden and nonprofit organization funding reveals disparities in funding across cancer types. Journal of the National Comprehensive Cancer Network, 17(7), 849–854. https://doi.org/10.6004/jnccn.2018.7280
American Lung Association. (2014, April). Addressing the stigma of lung cancer. Retrieved March 8, 2020, from U.S. Dept. of Health and Human Services. (n.d.) https://www.lung.org/lung-health-diseases/lung-disease-lookup/lung-cancer/living-with-lung-cancer/how-to-talk-about-your-cancer/addressing-lung-cancer-stigma
Lesbian, gay, bisexual, and transgender health. Healthy People 2020. Retrieved March 8, 2020, from https://www.healthypeople.gov/2020/topics-objectives/topic/lesbian-gay-bisexual-and-transgender-health#31
U.S. Census Bureau. (2019, May 23). Who are the uninsured? Retrieved March 8, 2020, from https://www.census.gov/library/stories/2018/09/who-are-the-uninsured.html
Warshaw, R. (2017, October 31). Health Disparities Affect Millions in Rural U.S. Communities. Retrieved March 8, 2020, from https://www.aamc.org/news-insights/health-disparities-affect-millions-rural-us-communities
