Adult Cardiac Arrest Team Lead
When treating a patient in cardiac arrest the role of the Team Lead is critical to organizing and coordinating the treatments needed to provide the patient with the best chance of survival. As an effective team leader, you must recognize the condition and act quickly and efficiently to increase the chances of survival.
Once cardiac arrest is identified, your responsibility as Team Leader is to ensure that the correct priority treatments are accomplished, either through delegation if you have sufficient team members, or by you directly if you don’t have resources to delegate. The high priority treatments during a cardiac arrest include the list below, however the first two treatments below (CPR and AED) are the most critical:
- Chest Compression task* – delegate to a team member (or better yet, two team members if you have the resources), ensure that high quality compressions are being performed and only stop compressions when the AED advises the team to do so. Also, if your resources allow, switch the team member performing compressions every time the AED advises you to stop compressions for a rhythm check (about every 2 minutes).
- Apply the Automated External Defibrillator (AED)
- Request your dispatcher to send an ALS response unit code three to your location and let them know CPR is in progress
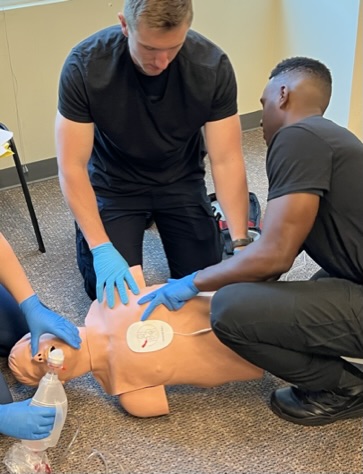
- Airway task
- History – Look for a DNR / POLST, find and write down the medications
- Think of possible causes of the cardiac arrest that might be reversible (Hs and Ts)
- If an ALS crew is enroute to assist you, prepare to give a brief summary hand-off report to the crew upon their arrival. Keep if brief and targeted by focusing only on the high-level details including:
- How you found the patient (example: Pt found down upon our arrival).
- Estimated time down without CPR being performed (if known).
- If a bystander was doing CPR when you arrived (example: daughter was performing CPR upon our arrival).
- Where you are in your cardiac arrest management (example: we’ve currently working on our 3rd round of CPR. The AED shocked on the first round and advised no shock on the second round. We do not have an airway placed yet and we are currently asking about a DNR or POLST form).
- Would you like to take PIC and how can I help you?
*Note: high-performance CPR has been known to cause CPR induced consciousness (eye opening, purposeful movement, speech). Continue CPR and reassess pulses only when the AED advises, “no shock advised.”


Flowcharts are a helpful tool to visualize the concepts and decision making necessary within this set of skills. Unfortunately, due to copyright restrictions we are unable to provide them here.
The authors recommend you or your instructor find an up-to-date version of this flowchart from the American Heart Association. A simple web search on cardiac arrest algorithm AHA should do the trick. If you are viewing the online version of this lab manual, this link will take you to the AHA CPR algorithms.
|
Cardiac Arrest Team Lead |
1 |
2 |
3 (instructor) |
|
Initials |
|
|
|
The original copy of this book resides at openoregon.pressbooks.pub/emslabmanual. If you are reading this work at an alternate web address, it may contain content that has not been vetted by the original authors and physician reviewers.

