Obstetrics and Childbirth
Imminent delivery is a common reason for requesting aid. As a prehospital healthcare provider, one of the most important decisions you will make for a patient experiencing symptoms of an imminent delivery is the decision to transport for a hospital delivery or to assist the mother with delivery of the baby on scene.
Decision to deliver:
Before we can make this decision, there are several questions that help us determine the proper treatment and none should be rushed. After scene safety, our next priority is to quickly establish a rapport with the patient. We will need to do some invasive examinations and expose the patient’s body in a very vulnerable way.
Try saying this out loud:
“Hello, my name is I am an EMT. I am here to help you. What is your name?
I need to ask some questions to best take care of you.
-
-
- What is your due date?
- Are you currently having contractions?
- Do you feel the urge to push?”
-
If the patient has the urge to push, then continue with this…
“I know we have just met, but I’m here as a healthcare professional to help you through this process. I need to perform a visual exam to see if the baby’s head is crowning. I will not be inserting my fingers or hand into your vagina unless I absolutely must. Do you have any pain or pressure in your vaginal or rectal area?”
To perform the physical exam:
- Inform the patient and trusted bystander of the need for visual inspection.
- “I understand that you might be having your baby. I need to visually inspect for bulging of the perineum for evidence of the baby’s head.”
- Clear the room of unnecessary personnel and bystanders or move to a more private location (i.e., back of ambulance)
- Position patient semi-fowlers or fowlers, knees bent, feet apart.
- Drape a blanket or sheet over the abdomen and knees. Keep modesty a priority.
- Visualize, but do not touch the vagina.
Timing Contractions
Time contractions from the beginning of one to the beginning of the next. Contractions are considered frequent if they are less than 2 minutes apart and are lasting more than 1 minute.
Decision points
- If the patient is experiencing contractions at increasing intensity and duration and the interval between contractions is shortening, birth may be imminent.
- If you can see the baby’s head, on scene delivery of the baby is recommended.
- If no crowning is noted, transport is recommended.
- If any other part of the baby is presenting i.e., the arm, leg, buttocks, see Breech presentation for next steps.
- If the cord is presenting before the baby or alongside the presenting part of the baby, this is of the highest mortality rate and must be treated with emergent transport. See prolapsed cord for specific treatment plan.
Transport of a pregnant patient & avoiding supine hypotension syndrome
Pregnancy changes a person’s body to accommodate a growing fetus. The following are normal changes that occur during pregnancy:
- Increased respiratory drive. As the uterus grows to accommodate the growing fetus, pressure is placed onto the diaphragm making it harder for the patient to take a deep full breath. Quality of breathing becomes shallow and slightly increases as late term pregnancy progresses.
- Increase in heart rate. The increase in HR is to accommodate the normal increase in circulating blood volume.
- There may also be obvious and painful swelling of extremities: wrists, hands, ankles, feet.
- Position the pregnant patient on their left side. This is the safest position to reduce the risk of supine hypotensive syndrome. This position protects the inferior vena cava from compression that would decrease cardiac output and cause hypotension amongst other untoward and dangerous symptoms.
Preparing to assist a field delivery.
If the need to stay on scene and deliver is recognized, take the following steps to prepare for delivery:
- Don additional PPE including eye protection, gowns, face shield, booties, and gloves.
- Call for an additional unit, preferably ALS.
- Continue to ask SAMPLE, natal, and prenatal questions.
- The position the pregnant patient takes during labor can vary to meet the comfort or desire of the patient. Various positions can be and, in some cases, should be considered by providers, to assist with delivery. Traditional delivery, or semi-fowlers delivery, is not the only way to position a laboring patient.
- Ample space around the patient is recommended.
- Traditional positioning: sitting, supported at 450 angles, knees bent, feet apart, and glutes at edge of surface, unless on the floor.
- Patient’s partner or trusted companion should be positioned beside the patient, holding hands for comfort.
- Place sheets and incontinence pads under the buttocks.
- Have towels, warm blankets, and gauze nearby and accessible.
Assisting in field delivery
- Encourage short shallow breaths between contractions “butterfly breathing.”
- Encourage pushing at the peak of contractions.
- Place the palm of your hands on the crowning head of the baby and avoid adding pressure.
- Guide the baby out of the vaginal canal by directing the head downward until one shoulder is delivered.
- Next, gently lift the baby either up or down to allow the second shoulder to deliver.
- Baby will be slippery! Maintain a gentle but firm grasp!
- Using a towel or blanket, rub the baby dry and stimulate. This will encourage a vigorous baby. Continue to stimulate and warm. These two actions are extremely important in acclimating the newborn.
- If the baby has little to no crying and is taking longer to acclimate, then consider suction using a bulb syringe. Suction the mouth and then the nostrils. Remember, NOT ALL babies need suctioning. Most of the amniotic fluid is forced from the mouth and nose as the baby’s chest is compressed during descent through the vaginal canal. This is nature’s way of clearing the oropharynx and nasopharynx of fluid.
- Place baby skin to skin with the parent. Encourage suckling. Continue to wipe the outside of the baby’s mouth to clear secretions and remember to warm, warm, warm the baby. Warming the baby is a necessary and mandatory intervention.
Continue to Post Delivery Care
Nuchal Cord Care
A nuchal cord occurs when the umbilical cord is wrapped around the neck of the baby during delivery. This can prevent exchange of oxygen by tamponading blood flow through the umbilical cord as well as preventing the neonate from breathing or crying through asphyxiation.
- When a nuchal cord is identified, slide fingers between the cord and neck of the neonate and gently pull the cord over the head.
- Proceed with delivery as indicated.
Prolapsed Cord care
If a prolapsed cord is present, assess the cord for pulsation. If the umbilical cord is pulsating, discourage the mother from pushing, wrap the cord in damp gauze, transport emergently to the nearest facility capable of performing a cesarian section and continually reevaluate for the presence of umbilical pulse.
If the umbilical cord has no pulse
- Place mother on her knees and elbows with her buttocks in the air.
- With a gloved hand, place 2 -3 fingers in the vaginal canal.
- Using the palm side of your gloved hand puts pressure on the neonate’s head.
- As you find the head reach about the head to feel for the cord.
- Slightly manipulate the head off the cord until pulses return.
- Leave your gloved fingers inserted in this position to allow for pulses to continue in the umbilical cord.
- Have team members apply saline soaked dressing to the prolapsed cord which is presenting out of the vaginal opening.
- Transport in that position code 3 to the nearest appropriate facility.
Post Delivery Care
- If the baby is not breathing once warm and dry you will need to continue rubbing the baby’s back and perhaps flicking the soles of their feet.
- After 1 – 3-minutes, place 1 clamp on umbilical cord 6-8 inches away from baby
- Place a second clamp ~2 inches distal from the first clamp.
- Once the cord has no pulse, use the scalpel to cut the cord in between the two clamps.
- Cord can be cut emergently once umbilical clamps are on, if and only if mother or baby are in distress. Otherwise, there is no rush to cut the cord until the baby has vigor. Remember to keep the baby at peri-level or pelvic level until the cord is cut.
- You now have 2 patients with the birth of the neonate.
- Split the EMS team into 2 teams.
- 1 team assessment and treatment of mother.
- 1 team assessment and treatment of neonate/s.
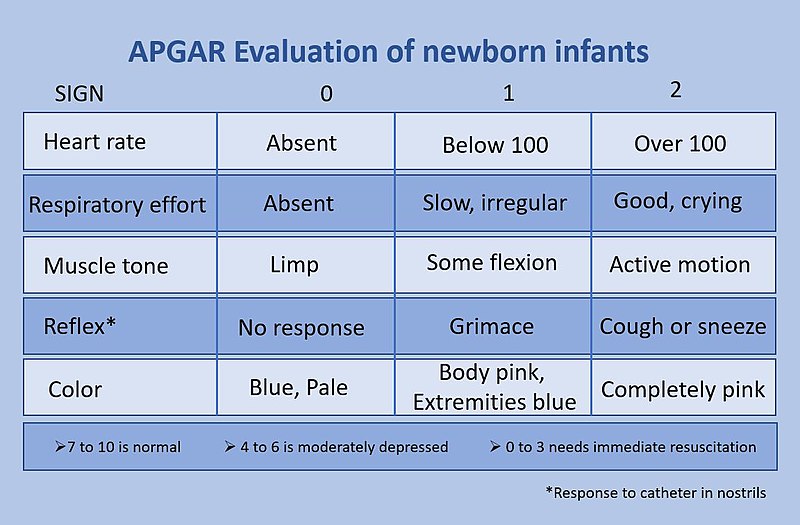
- APGAR (see attached guide) at birth and again at 5 minutes.
- Birthing patients will continue to have mild contractions as they prepare to deliver the placenta typically within 5 -15 minutes.
- If there is significant vaginal bleeding from the vagina, use fundal massage and if possible, encourage suckling.
- To perform fundal massage, place the palm of your hand on the fundus of the uterus, just below the umbilicus.
- Massage in very firm downward pressure and circular motion until bleeding slows.
- Call for ALS assistance.
- After delivery of the placenta, check for completeness of placenta. Any tears or pieces missing should be placed in a plastic bag and taken to the hospital.
|
Childbirth |
1 Student (normal) |
2 Student (abnormal) |
3 Student (abnormal) |
Instructor (Signoff) |
|
Initials |
|
|
|
|
The original copy of this book resides at openoregon.pressbooks.pub/emslabmanual. If you are reading this work at an alternate web address, it may contain content that has not been vetted by the original authors and physician reviewers.

