Introduction to Bone Health
The human skeleton consists of 206 bones and other connective tissues that together support and protect many organs, produce red and white blood cells, and act as a storage depot for minerals such as calcium, phosphorus, and magnesium. Although bones may look inactive at first glance, they are living tissues that are dynamic and in a constant state of breaking down and rebuilding to withstand mechanical forces. Bones also contain a complex network of canals, blood vessels, and nerves that allow for nutrient transport and communication with other organ systems.
Nutrition influences all body systems, and the skeletal system is no exception. Our lifestyle choices impact the health of our bones. In this section, we will look at how bone forms across the lifecycle and discuss the complex interactions of nutrients, hormones, genetics, and environmental factors that impact bone health.
What Is Bone?
Bone is a living tissue, made mostly of collagen, a protein that provides a soft framework, and minerals like calcium phosphate that form tiny crystals (called hydroxyapatite) around the collagen fibers. These inorganic minerals harden the collagen framework and provide strength. The combination of collagen and minerals makes bone both flexible and strong, which allows it to withstand stress.
Most bones contain two types of tissue, compact and spongy tissue, but their distribution and concentration vary based on the bone’s function. Spongy bone (also known as trabecular bone) is 50 to 90 percent porous and appears as a lattice-like structure under a microscope. It makes up about 20 percent of the adult skeleton and is found at the ends of long bones, in the cores of vertebrae, and in the pelvis, as it supports shifts in weight distribution. Compact bone (also known as cortical bone) is dense so that it can withstand compressive forces. It is only 10 percent porous, and it looks similar to the rings in a tree trunk, with many concentric circles sandwiched together. Compact bone tissue makes up approximately 80 percent of the adult skeleton and surrounds all spongy tissue.
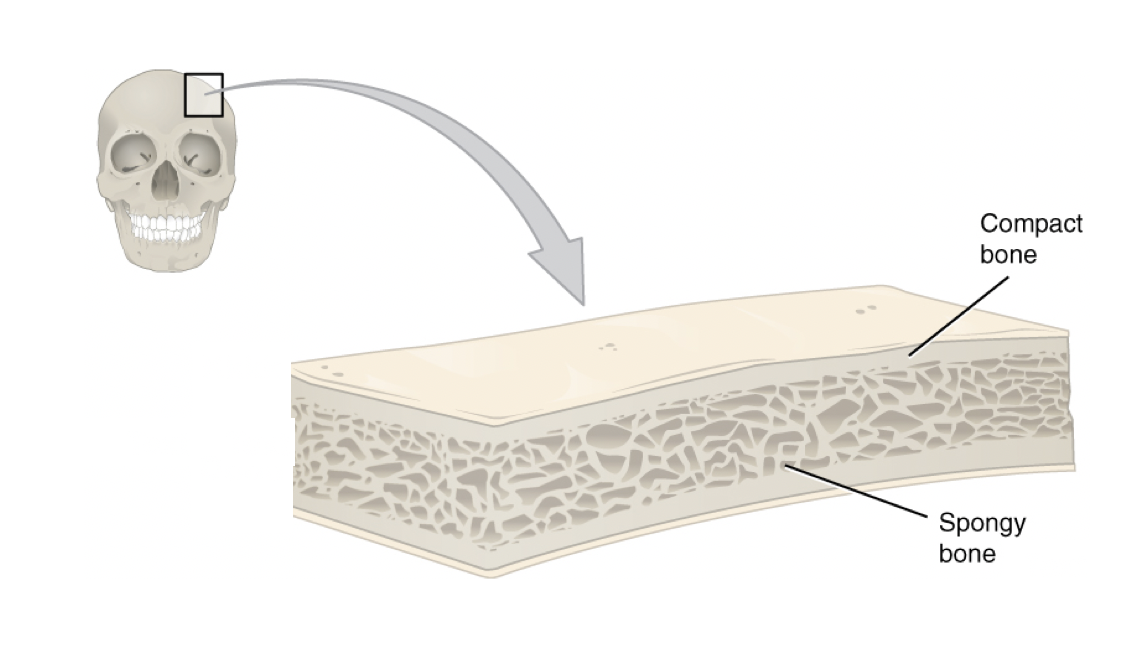
Figure 9.1. This cross-section of a flat bone from the skull shows the spongy bone lined on either side by a layer of compact bone.
Bone Growth, Modeling, and Remodeling
Bones change in shape, size, and position throughout the life cycle. During infancy, childhood, and adolescence, bones are continuously growing and changing shape through two processes: growth (or ossification) and modeling. In the process of modeling, bone tissue is dismantled at one site and built up at a different site, which influences the shape of the bone. During childhood and adolescence, more bone is deposited than dismantled, so bones grow in both size and density, reaching 90 percent of peak bone mass by age 18 in girls and age 20 in boys.2 Peak bone mass is reached by age 30, at which point bones have reached their maximum strength and density. Factors affecting peak bone mass include sex, race, hormones (e.g., estrogen and testosterone), nutrition (e.g., calcium and vitamin D intake), physical activity, and behavioral factors like smoking. These factors will be discussed in more detail when we discuss osteoporosis.
In adulthood, our bones stop growing and modeling, but they continue to go through a process of bone remodeling, in which bone tissue is degraded and built up at the same location. About 10 percent of bone tissue is remodeled each year in adults. Bones adapt their structure to the forces acting upon them, even in adulthood. This is why physical activity increases bone strength, especially when it involves weight-bearing activities. For example, tennis players can have measurably higher bone mass in the arm they use for play compared with the other arm.3 Ultimately, bones adapt their shape and size to accommodate function.
The dynamic nature of bone means that new tissue is constantly formed, and old, injured, or unnecessary bone is dissolved for repair or for calcium release. The cell type responsible for bone resorption, or breakdown, is the osteoclast. Osteoclasts are continually breaking down old bone tissue. Another type of cell, called osteoblasts, are continually forming new bone. The ongoing balance between osteoblasts and osteoclasts is responsible for the constant but subtle reshaping of bone. The decline in bone mass after age 40 occurs because the rate of bone loss is greater than the rate of bone formation. This means that osteoclast-mediated bone degradation exceeds that of the bone-building activity of osteoblasts. How much bone is lost in adulthood depends on peak bone mass reached in early adulthood and other risk factors, as we’ll discuss next.
Osteoporosis
Osteoporosis is a bone disease that occurs when bone density or bone mass decreases. The bone becomes thinner and more porous and is therefore more susceptible to breaking. According to the National Institute of Arthritis and Musculoskeletal and Skin Diseases, more than 53 million people in the U.S. either have osteoporosis already or are at high risk of developing it due to low bone mass.1
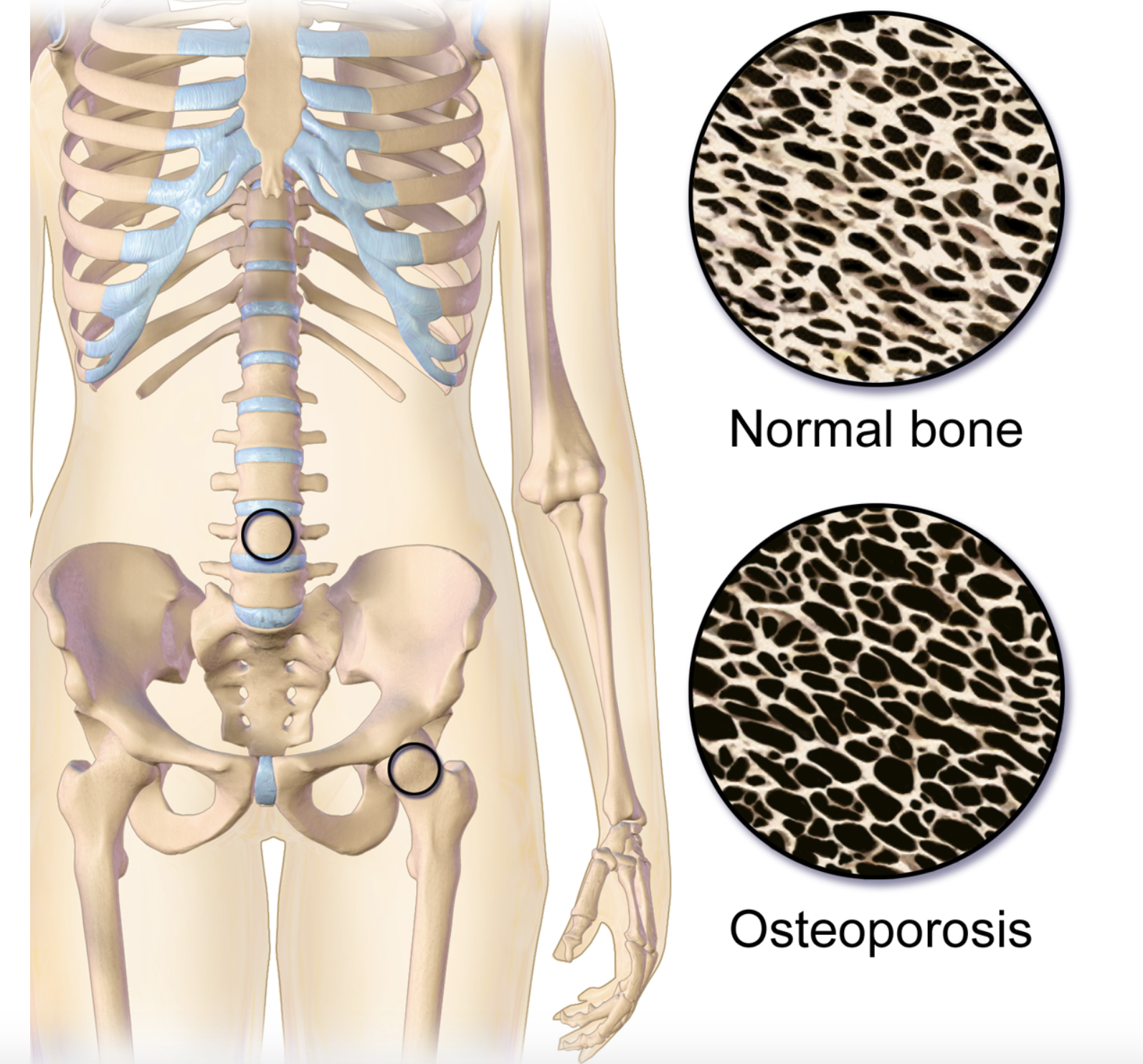
Figure 9.2. Osteoporosis. This illustration shows the difference between the structure of normal bone, which is less porous, and bone with osteoporosis, which is more porous. The two circles located on the spine and hip represent the location of the images.
Bone loss usually occurs without symptoms, so osteoporosis is often called a silent disease. It can go undetected until bones become so weak that they fracture due to a sudden strain, bump, or fall.
One way bone health can be assessed is by measuring bone mineral density. A bone mineral density (BMD) test can detect osteoporosis and predict the risk of bone fracture. The most common tool used to measure BMD is called dual energy X-ray absorptiometry (DXA). This method can measure bone density over the entire body, but most often the DXA scan focuses on measuring BMD in the hip and the spine. These measurements are then used as indicators of overall bone strength and health. DXA is painless, non-invasive, uses low doses of radiation, and is the most accurate way to measure BMD.
An individual’s chances of developing osteoporosis depend on several risk factors, some of which are controllable and some of which are not. It is thought that genetic factors (such as sex and race) may account for up to 75 percent of bone mass, and lifestyle factors (such as diet and exercise habits) account for the remaining 25 percent.2
Osteoporosis risk factors that are biological and can’t be controlled:
- Body frame size- People with small frames are at higher risk for osteoporosis.
- Race- Caucasian and Asian populations are at higher risk of osteoporosis compared to African American and Hispanic populations, which are at lower risk.1
- Family history– Having a family member with osteoporosis may increase risk, as heredity seems to play a part in the development of osteoporosis.
- Age- After age 40, bone mass declines due to bone breakdown exceeding bone formation. Therefore, any person over the age of 40 has an increased likelihood of developing osteoporosis compared with a younger person. Starting out with a higher peak bone mass in early adulthood enables you to lose more bone during the aging process and not develop osteoporosis.
- Sex- Females, on average, have a lower peak bone mass compared with males (see Figure 9.3) and a much greater risk of developing osteoporosis, in part because of hormone levels.
- Hormones- The female hormone estrogen and the male hormone testosterone both help to increase peak bone mass. Estrogen is the primary female reproductive hormone, and it stimulates bone building and reduces bone breakdown. When women go through menopause (usually around age 50), they experience a natural decline in estrogen levels, which accelerates bone loss and increases the risk of developing osteoporosis (Figure 9.3).
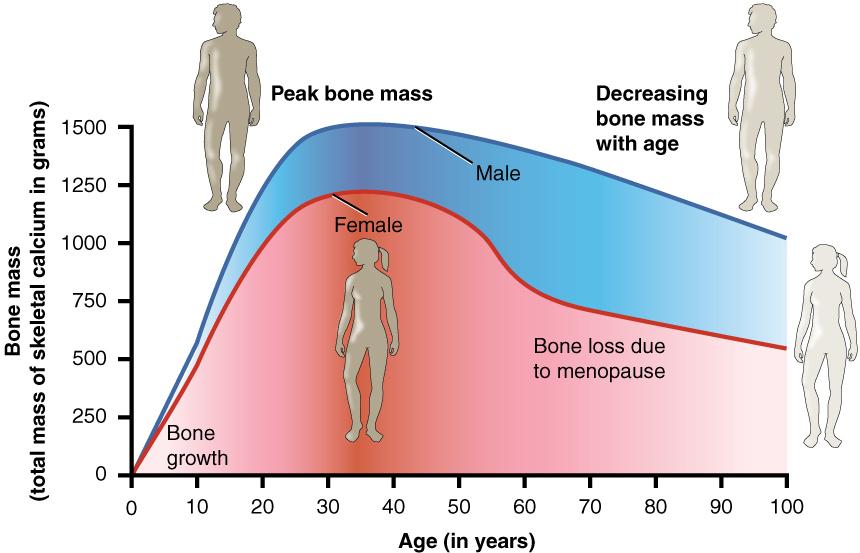
Figure 9.3. Age and bone mass. Bone density peaks at about 30 years of age, and women lose bone mass more rapidly than men, particularly around menopause.
Risk factors that can be controlled:
- Physical inactivity- Physical inactivity lowers peak bone mass, decreases BMD at all ages, and is linked to an increase in fracture risk, especially in the elderly. Regular exercise can help individuals achieve greater peak bone mass, prevents bone loss for women and men age 30 and older, and maintains strength and balance to help prevent falls later in life. The best activities for stimulating new bone are weight-bearing exercise, such as walking, hiking, and dancing, and resistance exercises like weight lifting.
- Nutrition- Ensuring adequate nutrition is a key component in maintaining bone health. Having low dietary intakes of calcium and vitamin D are strong risk factors for developing osteoporosis. Protein is also important during childhood and adolescence for proper bone development, and in older age to preserve bone mass.4
- Smoking- Smoking cigarettes has long been known to correlate to a decrease in bone mass and an increased risk of osteoporosis and fractures. However, because people who smoke are more likely to be physically inactive and have poor diets, it is difficult to determine whether smoking itself causes osteoporosis. Smoking is also linked to earlier menopause, and therefore the increased risk of developing osteoporosis among female smokers may also be attributed, at least in part, to having reduced estrogen production at an earlier age. However, studies have also shown that tobacco smoke and nicotine can directly impact bone metabolism.5
- Alcohol intake- Alcohol intake may also affect bone health, although this seems to depend on the amount consumed. Light to moderate alcohol intake (two drinks or less per day) has been shown in some studies to be associated with an increase in bone density and a decreased risk of developing osteoporosis. However, excessive alcohol intake is associated with decreased bone density and increased fracture risk, although this may be due in part to other lifestyle factors, such as poor diet and less physical activity.6
- Being underweight- Being underweight significantly increases the risk of developing osteoporosis, because people who are underweight often have a smaller frame size and a lower peak bone mass. The most striking relationship between being underweight and bone health is seen in people with anorexia nervosa. Anorexia nervosa is strongly correlated with low peak bone mass, and more than 50 percent of men and women who have this illness develop osteoporosis, often very early in life.
The changeable risk factors for osteoporosis provide ways for people to improve their bone health, even though some people may be genetically predisposed to the disease. Prevention of osteoporosis begins early in life since this is a critical time of bone growth. Eating a balanced diet that provides adequate amounts of calcium, vitamin D, and protein is important for bone health throughout the life cycle. Participating in exercise such as walking, hiking, and weight lifting, and refraining from risky behaviors like smoking and excessive drinking are all behaviors that will help protect bones.
Self-Check:
Attributions:
- Zimmerman, M., & Snow, B. Bone Structure and Function. In An Introduction to Nutrition (v. 1.0). https://2012books.lardbucket.org/books/an-introduction-to-nutrition/index.html, CC BY-NC-SA 3.0
- “Bone Tissue and the Skeletal System,” unit 6 from J. Gordon Betts, Kelly A. Young, James A. Wise, Eddie Johnson, Brandon Poe, Dean H. Kruse, Oksana Korol, Jody E. Johnson, Mark Womble, Peter DeSaix, Anatomy and Physiology, CC BY 4.0
Resources:
- 1National Institute of Arthritis and Musculoskeletal and Skin Diseases. Osteoporosis Overview. Retrieved April 22, 2020 from https://www.bones.nih.gov/health-info/bone/osteoporosis/overview
- 2National Institute of Arthritis and Musculoskeletal and Skin Diseases. Osteoporosis: Peak Bone Mass in Women. Retrieved April 22, 2020 from https://www.bones.nih.gov/health-info/bone/osteoporosis/bone-mass
- 3Kontulainen S., Sievanen H., Kannus P., Pasanen M., Vuori I. (2002). Effect of long-term impact-loading on mass, size, and estimated strength of humerus and radius of female racquet-sports players: a peripheral quantitative computed tomography study between young and old starters and controls. J Bone Miner Res 17: 2281–2289.
- 4International Osteoporosis Foundation. Nutrition. Retrieved April 28, 2020 from https://www.iofbonehealth.org/nutrition
- 5Al-Bashaireh, A. M., Haddad, L. G., Weaver, M., Chengguo, X., Kelly, D. L., & Yoon, S. (2018). The Effect of Tobacco Smoking on Bone Mass: An Overview of Pathophysiologic Mechanisms. Journal of osteoporosis, 2018, 1206235. https://doi.org/10.1155/2018/1206235
- 6Gaddini, G. W., Turner, R. T., Grant, K. A., & Iwaniec, U. T. (2016). Alcohol: A Simple Nutrient with Complex Actions on Bone in the Adult Skeleton. Alcoholism, clinical and experimental research, 40(4), 657–671. https://doi.org/10.1111/acer.13000
Images:
- Figure 9.1. “Anatomy of a Flat Bone” by J. Gordon Betts, Kelly A. Young, James A. Wise, Eddie Johnson, Brandon Poe, Dean H. Kruse, Oksana Korol, Jody E. Johnson, Mark Womble, Peter DeSaix, Anatomy and Physiology, OpenStax, licensed under CC BY 4.0
- Figure 9.2. “Osteoporosis” by BruceBlaus is licensed under CC BY-SA 4.0
- Figure 9.3. “Age and bone mass” by Anatomy & Physiology, Connexions Web site is licensed under CC BY 3.0
A protein important to the strength and structure of muscles, bones, tendons, ligaments, connective tissue, and skin.
Tiny crystals made from inorganic minerals that form around collagen fibers to provide strength to bones.
Also known as trabecular bone, this porous, lattice-like bone tissue makes up about 20 percent of the adult skeleton and is found at the ends of long bones, in the cores of vertebrae, and in the pelvis.
Also known as cortical bone, this dense bone tissue surrounds all spongy bone and makes up approximately 80 percent of the adult skeleton.
The process of building new bone.
Dismantling of bone tissue at one site and building up at another, changing the shape of the bone.
The point when bones have reached their maximum strength and density.
Degrading and building up of bone tissue at the same location.
The breakdown of bone.
The cells that are responsible for the breakdown of bone.
The cells that are responsible for building new bone.
A bone disease that occurs when bone density or bone mass decreases, becoming thinner, more porous, and more susceptible to breaking.
A test that can detect osteoporosis and predict the risk of bone fracture.
One of the most accurate but more expensive methods of measuring body composition; this method scans the body with low-dose X-ray beams to determine fat, muscle, and bone mass.

